Midclavicular to inframammary fold measurement, a method of evaluation for nipple sparing mastectomy
Introduction
Nipple sparing mastectomy (NSM) has been embraced as an oncologically safe technique to preserve the nipple areolar complex (NAC) for enhanced cosmesis in the carefully selected patient. Previously, we described oncologic and tissue characteristics of the ideal NSM candidate. To ensure adequate skin flap and nipple perfusion, large (>500 grams) and ptotic breasts are excluded from a single stage procedure (1). In patients with grade II or III ptosis (nipple below the level of the fold, or on the undersurface of the breasts, respectively) where the native NAC is of significance to the patient, we offer a staged procedure where mastopexy or reduction is performed before NSM (2). However, ptosis assessments may be equivocal and unreliable in some patients.
The objective of this paper is to describe a novel, simple method to determine tissue envelope characteristics. Specifically, we measure the length of the tissue envelope from the midclavicular line to inframammary fold (IMF). Similar to examining ptosis, this provides a metric that identifies an enlarged breast envelope and strained nipple perfusion. When an IMF incision is used, this measurement correlates to how far the perforators are able to extend to supply the NAC and the inferior mastectomy skin. Based on clinical experience, we hypothesized 34 cm to be the upper limit cut off where instead we offer a staged approach.
Methods
Our study is retrospective in nature with IRB approval. Inclusion criteria were NSMs completed by the senior surgeon via an inframammary approach (SCW) between 10/2010 to 7/2016. Our technique relies on creating flaps to achieve a thickness of >0.9 mm of the mastectomy flap. We routinely use sharp dissection avoid damaging the subdermal plexus on mastectomy flaps. Reconstruction was performed by three separate plastic surgeons operating in the same institution. All patients with NSM have ICG to help verify perfusion and after prosthetic devices are in place. Our algorithm tends to lean toward sub-pectoral expander reconstruction with acellular dermal matrix (ADM) for inferior implant support and prevention of window shading. Immediate implant reconstruction tends to be patient driven. We always counsel patients that it may not be possible if the mastectomy flaps will not support it. Two patients in this series received pre-pectoral reconstruction with complete ADM coverage of the prosthesis. For our chart review, we retrospectively examined patient characteristics, breast weight specimens, mid-clavicle to IMF length, and complications resulting. Patients were excluded for incomplete charts.
Measurement
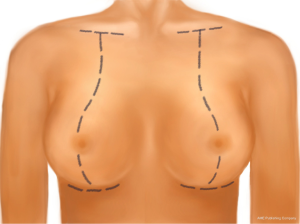
We perform our measurement during preoperative evaluation. The midclavicular point is identified half way between the sternal notch and the acromion. With the patient in the upright position, a measuring tape measures the distance along the breast meridian, from the midclavicular point to the IMF (Figures 1,2,3). The breast meridian is slightly laterally offset of the midclavicular line along its point of maximal projection. It accounts for the lateral nature of ptotic breasts. Nipples may be lateral to the breast meridian line in these ptotic breasts.
Statistics
We calculated descriptive statistics for the complication data and the entire data set. We used simple linear, binomial and ordinal logistic regression to assess associations between IMF to midclavicular measurement to breast weight, cup size and complication occurrences. A two-tailed value of P<0.05 was considered statistically significant. All statistical analyses were performed using SAS version 9.3 (SAS Institute, Inc., Cary, NC, USA).
Results
There were 59 patients with IMF approach NSM between 10/2010 to 7/2016. Twenty-one patients were excluded due to incomplete charts. Two were excluded because they had staged procedures prior to their NSM (n=36). The average age was 45 and body mass index (BMI) was 22. Half were performed due to cancer; the other half were prophylactic (BRCA1/2 =12). The majority underwent expander reconstruction (n=27), and the rest had immediate implant reconstruction (n=9). Five cases were performed unilaterally for a total of 67 breasts. Operated breasts were counted as separate units in statistical analysis. There were no smokers or patients previously irradiated in this series.
Data
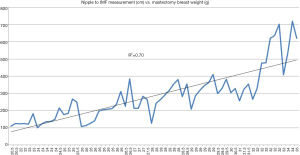
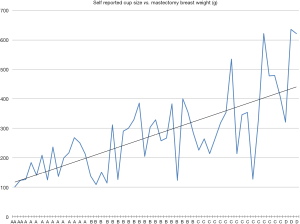
Examining the data, we found our mid-clavicle to IMF measurement to range from 20.5 to 35 cm with an average value of 27 cm. Individual patients had IMF to midclavicular measurements that varied between their right and left breasts, average difference was 0.6 cm with a range from 0 to 2 cm. Logistic regression analysis showed that increasing IMF to midclavicular measurement was significantly related to increasing breast weight in grams (R2=0.70, P<0.001) (Figure 4). Moreover, logistic regression analysis also showed that increasing bra cup size was significantly related to increasing breast weight in grams (R2=0.47, P<0.001) (Figure 5).
Complication rates were assessed in their relation to mid-clavicle to IMF measurements. Complication data were considered by analyzing each breast separately, given that measurements and complication rates vary independently between breasts. Complication data was analyzed by sorting data into two categories: no complications and complication present. Logistic regression analysis revealed that an increase in IMF to mid-clavicle measurement (expressed in cm) was associated with an increase in the odds of complication occurring with an odds ratio of 1.551 [Wald Χ2(1) =9.937, P=0.002]. Complications not related to ischemic mastectomy flaps, like capsular contracture and hematoma, were excluded in this analysis. Subsequently, complications were divided into three categories: none, minor and major. Minor complications included superficial, partial thickness, epidermal changes (skin wounds, epidermolysis) and minor ischemic changes. Major complications included frank necrosis/eschar development. Regression analysis was conducted to assess the relationship between increasing IMF to mid-clavicular measurements to ranked categorized complications. No significant relationship was found with this analysis.
Complications
Complication data are listed in Table 1. Overall, 13 of 36 patients (36%) or 15 of 67 breasts (22%, two bilateral) experienced a complication in the post-operative period. Three patients (8%) developed unilateral complications unrelated to mastectomy skin compromise (two hematomas and one capsular contracture). Three of the 36 patients (8%) or three of the 67 breasts (4%) experienced a complication that required a return to the operating room. Two patients [two breasts (3%)] developed post-operative hematomas that resolved with post-operative evacuation in the operating room. The last patient had frank necrosis requiring debridement.
Table 1
| Complications | Breasts [%] | Patients [%] |
|---|---|---|
| Ischemic skin changes, resolved without issue | 6 [9] | 4 [11] |
| Superficial epidermolysis | 2 [3] | 2 [6] |
| Frank necrosis, eschar formation | 4 [6] | 4 [11] |
Four patients [six breasts (9%)] developed ischemic skin changes around either the incision or the NAC. Four of these six breasts resolved on subsequent office follow up visits and two breasts (one patient) required hyperbaric oxygen therapy for resolution. These never progressed to epidermolysis of the skin. Four patients [four breasts (6%)] were found to have frank necrosis. Of these four patients, two patients required hyperbaric oxygen therapy, one patient required a return to the operating room for debridement of the nipple and one patient with frank necrosis had resolution on follow up visits with dressing changes. Two patients [two breasts (3%)] had superficial epidermolysis, both of which resolved at post-operative office visits, without explantation of reconstruction. One of these patients was the only >34 cm on one side in our series, whom we offered NSM after patient request. That particular patient had superficial epidermolysis of the breast with >34 cm measurement that resolved at 3 weeks. No explanations or infections requiring antibiotics occurred in this series.
Discussion
The first paper describing NSM by the senior author described anatomical exclusion criteria for NSM as excessive ptosis and large breast volume (>500 g) (1). Ptosis assessment may vary between observers. Furthermore, pseudoptosis, defined by the location of the nipple at the IMF and the majority of the breast below the IMF, will give lower ptosis measurements but subject patients with IMF NSM to the same number of complications due to the long length the blood supply must travel. The idea for the mid-clavicle to IMF distance was based on the concept that perforators of the breast envelope, particularly the second intercostal, must travel in the same direction in an IMF incision. Therefore, a simple quantifiable measurement affords accuracy and speed by which a decision can be made. Based on clinical experience, 34 cm has been the relative cut off for IMF incisions in NSM. Our necrosis rates with this protocol are on par with cited literature rates of 5.9% among 12,358 NSM (3). We demonstrate significantly increased complication rates when approaching 34 cm. Furthermore, we demonstrated a better correlation of mid-clavicle to IMF measurement with mastectomy weight compared to self-reported cup sizes. In this situation, surgeons should be wary and discuss with the plastic surgeon alternate incision and reconstructive options. Our use of intraoperative ICG perfusion studies ultimately guide intraoperative fill, and reconstruction to be a helpful adjunct to identify compromised skin flaps.
In situations where the mid-clavicle to IMF measurement is greater than 34 cm, we have found staging resection to be a viable option as previously described (2). We faced wound healing issues when one patient was >34 cm, although this resolved without loss of reconstruction. The procedure must be staged as flap necrosis, nipple malposition, and necrosis of the nipple are all serious issues. In coordination with plastic surgery, we perform a circumvertical or Wise-pattern skin reduction. The reduction is generally skin only or a small parenchymal reduction (<100 g) from a central inferior wedge. The NSM ideally occurs at least 10–12 weeks later when incisions are healed, chemotherapy completed, and immune function has returned. In therapeutic mastectomies, the guiding principle in the patient with a diagnosis of breast cancer is that the tumor is removed entirely with clear margins as is done for breast conservation therapy. This is intended to be identical or analogous to the patient undergoing breast conservation therapy with oncoplasty. The key difference is that the mastectomy comes later rather than radiation therapy.
Ultimately, distance the vessels have to travel is one component of what makes a successful reconstruction. Mastectomy flap thickness, trauma to the mastectomy flap, and pressure from the reconstruction impeding inflow all work in synchrony to determine the ultimate surgical outcome. To our knowledge, this is the first paper to demonstrate the mid-clavicle to IMF distance as an objective measurement to help guide IMF NSMs. We are able to demonstrate this measurement correlates with mastectomy weights. Further, increasing measurements were correlated with increasing mastectomy complications. We believe this simple tool will be a valuable addition to the breast and plastic surgeon alike.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/abs.2018.01.01). TAP is on the speaker bureau for Novadaq. The other authors have no conflicts of interest to declare that pertain to the contents of this manuscript.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Our study is retrospective in nature with IRB approval. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Spear SL, Willey SC, Feldman ED, et al. Nipple-sparing mastectomy for prophylactic and therapeutic indications. Plast Reconstr Surg 2011;128:1005-14. [Crossref] [PubMed]
- Spear SL, Rottman SJ, Seiboth LA, et al. Breast reconstruction using a staged nipple-sparing mastectomy following mastopexy or reduction. Plast Reconstr Surg 2012;129:572-81. [Crossref] [PubMed]
- Headon HL, Kasem A, Mokbel K. The oncological safety of nipple-sparing mastectomy: a systematic review of the literature with a pooled analysis of 12,358 procedures. Arch Plast Surg 2016;43:328-38. [Crossref] [PubMed]
Cite this article as: Fan KL, Graziano FD, Abbate O, Pittman TA, Willey SC. Midclavicular to inframammary fold measurement, a method of evaluation for nipple sparing mastectomy. Ann Breast Surg 2018;2:3.