
Visual assessment of scapular position following delayed breast reconstruction with the latissimus dorsi flap or the thoracodorsal artery perforator flap
Introduction
The pedicled myocutaneous latissimus dorsi (LD) flap is often used as a secondary choice for delayed breast reconstruction, when the deep inferior epigastric artery perforator (DIEP) flap cannot be used. The LD flap can be harnessed for total autologous breast reconstruction in patients with a high body mass index or in combination with an implant when additional volume is required (1).
The LD muscle acts as a powerful extensor and adductor of the shoulder with an additional effect on internal rotation of the humerus and downward rotation of the scapula (2). The muscle plays an important role for maintaining dynamic stability of the shoulder joint by keeping the humeral head in the glenoid fossa (3). Shoulder morbidity may occur following harvest of the LD muscle for reconstructive purposes due to loss of both muscle function and its stabilizing role (4,5).
The thoracodorsal artery perforator (TAP) flap is used as a muscle sparing alternative to the LD flap for delayed breast reconstruction. The flap is based on a skin island raised on perforators from the thoracodorsal artery (6,7). The use of the TAP flap leaves the LD muscle function intact and the possible associated muscle related morbidity may not occur (8). We do not know if the use of the LD muscle affects the position of the shoulder joint and/or the scapula.
The aim of this study was to develop a method for photographic assessment of the back and position of the scapula following delayed breast reconstruction using the LD flap or the TAP flap and to examine if there was any difference between the position of the scapula between groups.
Methods
We conducted a retrospective study as an amendment to an on-going PhD-study. Participants were recruited from one of the existing cohorts in the PhD-study including women who previously had a delayed breast reconstruction by either the LD flap (25 patients) or the TAP flap (24 patients) in the period between January 1st 2009 and August 31st 2013, at the Department of Plastic Surgery, Lillebaelt Hospital, Vejle, Denmark.
The study was approved by The Regional Committee of Health Research Ethics for the Region of Southern Denmark and photo recordings were obtained at the outpatient clinic at the department.
Photography
The photos were recorded by a professional clinical photographer at Lillebaelt Hospital. One room was designated for the photo recording and arranged in a standardized setting: the camera (Canon EOS 5D Mark III) was placed on a tripod at a height of 125 cm at a 90-degree angle to the floor. The patient position was marked on the floor 150 cm from the camera. Each patient stood in an upright position, parallel feet at a T-shaped marking with the back towards the camera. The acromion and the inferior angle of the scapula (AI) were identified and marked with 15 mm Styrofoam balls.
Photographic analysis
The photographic analysis was carried out by one examiner blinded to patient related data and group allocation. The photographs were analysed in the software program PhysioEasy®, using measurements of angles and relative distances (measured in pixels) from tracing lines of the anatomical points.
Assessment of scapular deviation
The objective of the photo analysis was to assess if it was feasible to develop a method for visualizing and scoring the position of the AI relative to the thoracic columna. The data from the photo analysis is shown in Figure 1. The angles, AB and CB, were calculated using the software program. We then used the reverse angles, rAB and rCB to obtain positive scores with increasing inferior and lateral displacement of the AI.
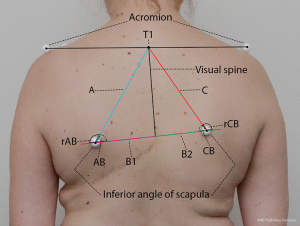
The score was calculated for each side by adding the distance from T1 to the AI (A or C) and the distance from the visual spine to the AI (B1 or B2), divided by the reverse angle (rAB or rCB). The resulting scores were then divided by 100 to make them more applicable for comparison between groups. We calculated a score for the operated side (Sop) and the non-operated side (Snop). Furthermore, we calculated a within-subject difference (Sdiff) between the Sop and Snop. We used an unpaired t-test to investigate the difference in Sop, Snop and Sdiff between the two groups. We used a Student’s t-test to investigate the within-group difference between Sop and Snop. All data are presented as mean ± standard deviation (SD), and statistical significance level is set at P≤0.05.
Results
Forty-nine patients were invited to participate in the study, of which thirty-three women aged 38 to 71 years, 16 LD and 17 TAP, accepted the invitation.
Scapular asymmetry
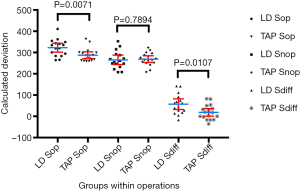
The calculated score revealed a significant within-group difference between the Sop and Snop for both operated groups, LD: Sop =322.6±9.8 and Snop =265.4±10.4, P<0.0001 and TAP: Sop =287.4±7.4 and Snop =268.8±7.4, P=0.04). Overall, there was a significant difference between the position of the scapulae in the two groups (LD: 57.2±11.6, TAP: 18.6±8.3, P=0.0107). More importantly, there was a significant difference between the position of the scapulae in the two groups on the Sop (LD: 322.6±9.8, TAP: 287.4±7.4, P=0.0071), but there was no difference between the Snop (LD: 265.4±41.8, TAP: 268.8±30.6, P=0.7894) (Figure 2).
Discussion
We assessed the position of the scapula through photo analysis and found a significant difference between the degree of displacement of the AI between women operated with the LD flap and the women operated with the TAP flap. The AI deviated significantly more laterally/anteriorly on the Sop of the LD reconstructed patients compared to the TAP reconstructed patients (Figure 3).

Until now, the studies investigating donor site morbidity following breast reconstruction with the LD flap have reported on outcomes such as pain, range of motion (ROM) and strength of the ipsilateral shoulder (4). The findings of this study on scapular positioning imply that harvesting the LD muscle for reconstructive purposes affects the position of the ipsilateral scapula. This could be a result of a loss of stabilization of the shoulder, which the LD muscle provides (3,9).
The increase of scapular asymmetry in patients having LD flap reconstruction, though not indicative of shoulder impairment, may imply a detrimental biomechanical effect of harvesting the LD muscle. This is in agreement with other studies concerned with donor site morbidity, which shows a decline in the strength and active ROM of the ipsilateral shoulder following the LD flap procedure (4,5).
The applied method using clinical photographs for assessing postural indices is well studied and can provide a low-cost, and easy to use tool for detecting visual biomechanical changes (10). However, the generation of a single score to represent scapular positioning might misrepresent the actual state of asymmetry of the scapulae. Although the process of postural assessment using photographs has been validated and found reliable for the indices as used in this study (11,12), this current method and the ability to detect changes over time for these indices, has not.
This study is hypothesis generating, which shows that the method for assessment of scapular position is feasible and that the scapular position seems to be more affected on the Sop of the patients reconstructed by the LD flap. However, the study is limited by the fact that we do not have any preoperative data regarding the position of the scapular prior to surgery from the two groups. In theory, although doubtful, the difference between groups could have been present prior to surgery.
The perspective of assessing the position of the scapula in the two groups could be to examine if there is an association between the position of the scapula and the degree of patient experienced morbidity for instance shoulder and arm related morbidity following reconstruction of the breast using a skin island from the back.
Conclusions
We tested, developed and found a feasible method for assessing the position of the scapula in women undergoing delayed breast reconstruction with a skin island from the back. There was a significant deviation of the scapula in patients reconstructed by the LD flap compared to the TAP flap, which may signify that the harvest of the LD muscle may influence the position of the scapula, the glenoid fossa and the position of the shoulder joint.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/abs.2018.01.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by The Danish Committee on Health Research Ethics as well as the Danish Data Protection Agency (ID: S-20120207) and in accordance with the Helsinki Declaration. Informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Schneider WJ, Hill HL Jr, Brown RG. Latissimus dorsi myocutaneous flap for breast reconstruction. Br J Plast Surg 1977;30:277-81. [Crossref] [PubMed]
- Bogduk N, Johnson G, Spalding D. The morphology and biomechanics of latissimus dorsi. Clin Biomech (Bristol, Avon) 1998;13:377-85. [Crossref] [PubMed]
- An KN. Muscle force and its role in joint dynamic stability. Clin Orthop Relat Res 2002;S37-42. [Crossref] [PubMed]
- Lee KT, Mun GH. A systematic review of functional donor-site morbidity after latissimus dorsi muscle transfer. Plast Reconstr Surg 2014;134:303-14. [Crossref] [PubMed]
- Forthomme B, Heymans O, Jacquemin D, et al. Shoulder function after latissimus dorsi transfer in breast reconstruction. Clin Physiol Funct Imaging 2010;30:406-12. [Crossref] [PubMed]
- Angrigiani C, Grilli D, Siebert J. Latissimus dorsi musculocutaneous flap without muscle. Plast Reconstr Surg 1995;96:1608-14. [Crossref] [PubMed]
- Jacobs J, Børsen-Koch M, Gunnarsson GL, et al. The Versatile Extended Thoracodorsal Artery Perforator Flap for Breast Reconstruction. Ann Plast Surg 2016;77:396-400. [Crossref] [PubMed]
- Hamdi M, Decorte T, Demuynck M, et al. Shoulder function after harvesting a thoracodorsal artery perforator flap. Plast Reconstr Surg 2008;122:1111-7; discussion 1118-9. [Crossref] [PubMed]
- Campbell ST, Ecklund KJ, Chu EH, et al. The role of pectoralis major and latissimus dorsi muscles in a biomechanical model of massive rotator cuff tear. J Shoulder Elbow Surg 2014;23:1136-42. [Crossref] [PubMed]
- Rosário JL. Biomechanical assessment of human posture: a literature review. J Bodyw Mov Ther 2014;18:368-73. [Crossref] [PubMed]
- Engsberg JR, Lenke LG, Bridwell KH, et al. Relationships between spinal landmarks and skin surface markers. J Appl Biomech 2008;24:94-7. [Crossref] [PubMed]
- Ferreira EA, Duarte M, Maldonado EP, et al. Postural assessment software (PAS/SAPO): Validation and reliabiliy. Clinics (Sao Paulo) 2010;65:675-81. [Crossref] [PubMed]
Cite this article as: Rommedahl MR, Rindom MB, Thomsen JB, Sørensen JA. Visual assessment of scapular position following delayed breast reconstruction with the latissimus dorsi flap or the thoracodorsal artery perforator flap. Ann Breast Surg 2018;2:5.

