An algorithm for the management of tuberous breast deformity
Introduction
Tubular/tuberous breast deformity (TBD) has always been an aesthetic challenge to plastic and breast surgeons. The outcome is often dependent on several factors that contributes to the overall aesthetic appearance of the breast. These include the laterality (U/L vs. B/L), in addition to the type of deformity denoting the grade of severity as per von Heimburg’s classification (1). Treatment objectives usually aim to achieve symmetry, volume replacement, ptosis correction and nipple-areola complex (NAC) correction (2). However, no single technique is able to achieve all the above, and sometimes a combination of procedures is necessary in order to manage individual features and different clinical presentations. Therefore, the decision-making process is important in order to choose between a single or staged reconstruction depending on the severity of the deformity.
Surgical options varied over the past years with the majority of the described techniques focused on achieving all the treatment objectives in a single setting. With the development of new generation implants (3), and the advent of the permanent expander prostheses (4-6), the necessity for other surgical techniques has become less prominent in recent years. Sometimes complementary procedures may be necessary in a form of ipsilateral mastopexy, or a contralateral augmentation mammoplasty with or without mastopexy in order to achieve symmetry.
The concept of staged reconstruction for TBD was utilised in order to improve the aesthetic outcomes in more severe forms. They often require a two-stage procedure that starts potentially with tissue expansion (TE) followed by a second stage definitive implant (1,7). This could also include mastopexy, or other different combinations.
The option of a single stage or two-stage reconstruction is usually based on the surgeon’s subjective evaluation. To date, there is no single study that demonstrates a holistic treatment algorithm, which encompasses all the aforementioned factors and patient satisfaction in the treatment strategy of this complex anomaly. This study aims to propose a treatment algorithm that serves as a guide in managing this complex deformity.
Methods
This was a retrospective review of 96 TBD patients undergoing surgical correction covering a period of five years, between February 2004 and June 2009.
The hospital clinical governance board and audit department approved this study. There were no ethical implications and therefore an ethical approval was not required. The data obtained in this study did not involve any patient identifiable information or images and therefore consent was not necessary.
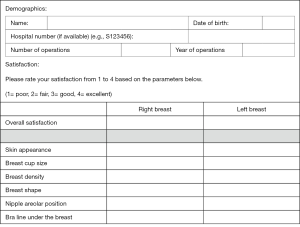
A number of evaluation criteria were obtained from patients’ clinical notes using a pre- designed data collection form (Figure 1). Preoperative evaluation criteria included standard breast measurements of suprasternal notch to nipple (SSN-nipple) distance, nipple to submammary fold (nipple-SMF) distance, nipple to midline distance (nipple-midline), breast base size, NAC size, bra size, grades of ptosis, and details of any scars.

Postoperative evaluation criteria included patients’ subjective grading of skin quality, breast volume, breast shape, nipple position, areola size, and the SMF. These were graded according to patient satisfaction using a validated four-point visual analogue scale (1= poor, 2= fair, 3= good, and 4= excellent) (8).
von Heimburg’s classification for TBD (1) were used to determine the grade of deformity for each patient. Patients were grouped according to their grades of deformity into two major groups: (I/II) and (III/IV). Patients with bilateral deformities who had different grades in each breast were classed according to the higher-grade breast, and therefore were categorised into the higher-grade group.
Patients were evaluated at one of their follow up visits following their surgery. They were then asked to evaluate their postoperative result, and to subjectively rate their satisfaction on a scale of one to four for each breast noting the aforementioned postoperative evaluation criteria. The scores from each breast were then averaged out in order to establish the overall satisfaction score for every patient.
The two groups were compared in terms of laterality, the choice of the surgical reconstruction whether it was a single stage or two-stage procedure, and the final patient satisfaction for their individual procedure. The comparison of patient satisfaction from each group in relation to their reconstructive procedure was analysed using a two-sample t-test in order to establish the significance in the difference between the single stage and two-stage procedures within each group.
All patients requiring ‘revisions’ following the completion of their reconstructive procedure were also evaluated as a separate subgroup. The reasons for revision were also correlated with both laterality, and the initial single or two-stage reconstructive procedure in order to compare the differences in each group.
In 2012, a follow up satisfaction questionnaire was sent out to all studied patients. This included the similar subjective evaluation criteria, as well as the same four-point satisfaction scale (Figure 2).
Results
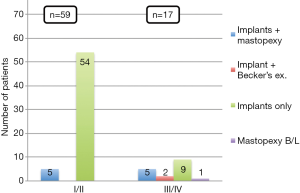
A total of 96 patients were identified who required surgical correction of their TBD. Two thirds of TBDs were classified into the lower grades group (I/II= 62 patients) and the rest were classified into the higher grades group (III/IV= 34) (Figure 3).
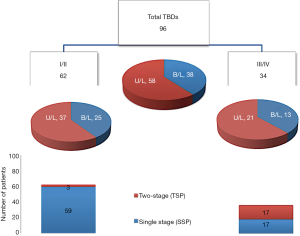
Approximately two thirds of TBDs were unilateral [58] and one third bilateral [38]. Similar distribution was observed for each of the two main groups with the lower grades (I/II) consisting of 37 unilateral vs. 25 bilateral. The higher grades consisted of 21 unilateral vs. 13 bilateral (Figure 3).
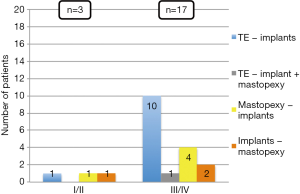
Patients in each group were divided into two subgroups depending whether reconstruction was staged or not. Majority of the patients, (95%, 59 patients) in the lower grade group required a single stage reconstruction, as compared to 3 patients (5%) having a two-stage reconstruction. The higher grades group had an equal distribution between the single and two-stage reconstruction with 17 patients (50%) each (Figure 3).
Seventy-six patients underwent a single stage reconstruction from both groups were analysed and demonstrated that implants-only based surgery was the most common procedure in both groups with 54/59 patients in the lower grades group compared to only 9/17 in the higher grades group. A combination of implants with mastopexy reconstruction was the second most common procedure with equal distribution between the two groups consisting of 5 patients each. Two patients only with bilateral deformity required a permanent implant in one breast and Becker’s expander prosthesis in the other one. Only one patient had bilateral mastopexy (Figure 4).
Twenty patients required a two-stage reconstruction. A first stage TE followed by a second stage implant replacement was the commonest procedure in the higher grades group comprising of 10/17 patients as compared to only 1/3 patient in the lower grades group. Mastopexy followed by implants was the second most common procedure with 4/17 patients in the higher grades group as opposed to only 1/3 patient in lower grades group. Two patients had initial implants with subsequent mastopexy in the higher grades group compared to only 1/3 patient in the other group. Only 1/17 patient had initial TE followed by a combination of implant replacement and mastopexy as a second stage in the higher grades group (Figure 5).
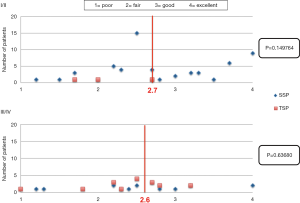
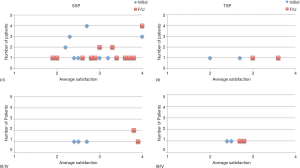
In the lower grades group, the overall mean satisfaction grade for those who required a single stage procedure was 2.7 [range, 1.2–4; standard deviation (SD), 0.7255]. Whereas, the remaining who required a two-stage procedure had an overall mean satisfaction grade of 2.1 (range, 1.7–2.7; SD, 0.51316). In the higher grades group, the overall mean satisfaction grade was 2.6 (range, 1.2–4; SD, 0.748381) for those requiring a single stage reconstruction, compared to 2.5 (range, 1–3.2; SD, 0.5525) for those undergoing a two-stage procedure.
An independent (unpaired) two-sample t-test was performed in order to establish if there is any difference in mean patient satisfaction scores between the single stage and the two-stage reconstruction within each group. The mean satisfaction score was not statistically significant between these two options for both groups (Figure 6). However, majority of patients rated an average score of 2.3 (range, 1.2–2.8), and a third achieved good to excellent result with an average score of 3.6 (range, 3–4).
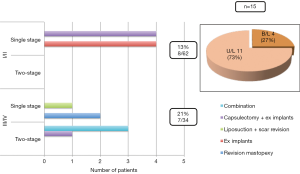
Out of the total number of patients, fifteen required revisional surgery. Three times as many revisions were performed in patients with a unilateral deformity (9) possibly because of the need to match the contralateral breast. The distribution of patients was almost equal in relation to the lower and higher grades (8 and 7 patients respectively). Following a single stage procedure, 8 patients from the lower grades group required revision because of capsule formation (4), or due to changes in the breasts with time and physiology (4). Seven patients from the higher grades required various revisions. These included mastopexy revision (2), capsulectomy and exchange of implants (1), contralateral breast liposuction and scar revision (1). Three patients required a combination of the above procedures (3). The overall revision rate was more common in the higher grades group 21% (7/34) compared to 13% (8/62) in the lower grade group (Figure 7). Apart from a number of minor incidences related to bruising, wound dehiscence as a result of either superficial infection or suture abscesses, in addition to skin striae following TE, there were no major complications recorded in our series during the time of follow up.
Mean follow up time from the first operation until last revision was two and half years (range, 6–48 months). The average time from the last follow up clinic until the completion of the satisfaction questionnaire was five years. Only 23 (24%) patients completed and returned the questionnaires. On average, patients remained satisfied with their result after an average period of 5 years with an overall mean satisfaction score 3.2 compared to the initial 2.8 following completion of reconstruction. However, due to the low response rate (24%) it was difficult to establish whether there was a significant change in patient satisfaction between a single or staged reconstruction (Figure 8). In addition to the 15 patients that required revisional surgery, two patients expressed their desire for NAC correction.
Discussion
The findings of this study demonstrate that TBD can be treated in either a single stage or two-stage without a difference in patient satisfaction with the outcome. It appears however that the single stage reconstruction has been the treatment of choice in the majority of cases. Implants only or in combination with mastopexy was predominately used in the lower grades group. A two-stage reconstruction may be advantageous in the higher grades and unilateral deformities as reflected in the high revision rate (21% and 73% respectively) (Figure 7).
It is already known that TBD is a complex anomaly. When the deformity is unilateral it is usually more difficult to achieve symmetry because the contralateral breast may also require correction. Whereas, being able to operate on both breasts simultaneously, in the bilateral deformity, gives more flexibility to achieve symmetry. This complexity has led to the development of a wide array of techniques and treatment plans throughout the literature. However, the key to achieve a satisfactorily aesthetic and symmetrical result is by implementing a treatment algorithm, in addition to understanding management principles. The main objectives to successfully treat this deformity are to achieve symmetry, ptosis correction, volume replacement and NAC correction (2).
There is no single study that refers to patient satisfaction in correlation with the grade of deformity, and whether it is unilateral or bilateral (laterality). Meara et al. (2) published similar findings from a small series of patients, whereby he illustrated a treatment algorithm based on a similar classification to von Heimburg’s (1). He treated type I breasts (i.e., grades I/II) with either an implant or mastopexy. Most of type II breasts (i.e., grade III) were treated with a combination of mastopexy and implants without a reference to whether this was performed in a planned two-stage, or as a revisional procedure. Type III (i.e., grade IV) required TE first before the placement of a permanent implant (2). Similarly, he reported that adjustments to the contralateral breast might be necessary in the unilateral deformities in order to achieve symmetry (2). This corresponds to the findings of this study that demonstrated a higher revision rate (73%) associated with unilateral deformities.
In a study reviewing patient satisfaction with the single stage augmentation with mastopexy, Spear et al. (8) highlighted a number of issues with regards to patients versus surgeon’s perception of the aesthetic outcome following a single stage reconstruction. Overall, patients were satisfied with the outcome, but the results were not consistent with the surgeons’ evaluation. It was suggested that achieving an excellent result was difficult, mainly because augmentation combined with mastopexy is a relatively complex procedure that carries the risks of both procedures. This may negatively influence both the patients’ and surgeons’ perception of the aesthetic outcome. The high rate of revisional surgery (54%) that was reported in Spear’s et al. study (8) highlights the complex nature of the combined procedure. Therefore, a two-stage procedure may not necessarily alter patient satisfaction with the outcome (8).
The importance of volume replacement and symmetry in TBD management was highlighted in a study by Persichetti et al. (10). The type of deformity according to Grolleau’s et al. (9) classification, and the degree of volume asymmetry largely influenced the choice of treatment in this study. Therefore, a single stage procedure was mainly used in mild to moderate asymmetry. This ranged from the application of glandular flaps to the use of permanent expandable implants in combination with mastopexy or reduction mammoplasty techniques. In contrast, severe volume asymmetry, particularly in the unilateral deformities, required a staged reconstruction by TE first followed by a placement of permanent implant later. Patient satisfaction with the shape, volume and symmetry of the breasts was assessed using a similar visual analogue scale (1= poor to 4= excellent), which demonstrated that all patients scored between good and excellent (10).
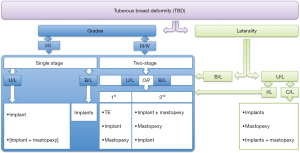
Published literature lacks a comprehensive algorithm that addresses both the grade or type of deformity and the issue of laterality in the planning of TBD treatment. It is already established that there is no perfect surgical technique that encompasses all the treatment objectives. Our findings confirm that patient satisfaction was not affected by the method of reconstruction. However, factors related to the laterality and the grade of deformity may influence the surgeons’ perception of the treatment plan. Therefore, a comprehensive treatment algorithm was proposed from the findings of this study (Figure 9).
This algorithm is based on the combination of the grade of deformity (I/II vs. III/IV) and laterality [unilateral (U/L) vs. bilateral (B/L)] in planning the reconstructive options for a patient with TBD. Therefore, for those patients with lower grades (I/II), the single stage procedure may be a better option, whereas a two-stage reconstruction may be more appropriate for the higher grades (III/IV). Because the bilateral deformity will require operating on both breasts simultaneously, it is possible to achieve the objectives with implants only in the lower grades, whereas a two-stage procedure may be required for the higher grades. The presence of a unilateral deformity adds some difficulty into management planning, because in addition to the affected ipsilateral breast, the normal contralateral breast also needs to be addressed to achieve symmetry. Therefore, as per the algorithm, the ipsilateral breast will follow the unilateral pathway by implementing either a single or two-stage procedure depending on the grades, whereas the contralateral breast might require a matching procedure in order to achieve symmetry (Figure 9).
This algorithm is proposed as a working guide for surgeons encountering this complex deformity. It is not a previously validated protocol, but it is based on a retrospective analysis of clinical experience and patient satisfaction with the outcome at our institution. We acknowledge that there are some limitations in this study. The surgeon’s personal evaluation could have been included, but that is subject to personal bias. Though an independent observer evaluation would have been ideal to compare the surgical outcome with patients’ own satisfaction score, it was difficult to implement this within a busy clinical set-up with time constraints on both patients and the evaluator.
In addition, the number of patients that completed the follow up satisfaction questionnaires was relatively low (24%), which did not enable the comparison of patient satisfaction scores after five years.
Due to the small number of patients in the revisional surgery subgroups, it was difficult to comment on the higher rate of revisions in the unilateral deformities and the higher grades in comparison with the bilateral and lower grade deformities. However, clinically it was felt that both ‘laterality’ and ‘severity of grade’ did contribute to the overall management of the difficult and varied clinical presentations of TBD.
Conclusions
TBD is a complex anomaly that poses a significant challenge to plastic surgeons due to the diversity of its features and the continuing uncertainty of its aetiology. Factors like laterality, and grades of deformity form an essential part of the assessment and treatment objectives. The surgical techniques for the correction of TBD are focused on achieving these objectives in majority of cases in a single stage. Higher grades may require a two-stage approach depending on the associated features and the laterality. It is, however, difficult to achieve symmetry particularly when the deformity is unilateral, and especially for those patients with higher grades.
This study showed that there was no significant difference in patient satisfaction between the lower and the higher grades. It was also evident that TBD can be treated in either a single stage or two-stage without affecting patient satisfaction with the outcome. The majority of patients had a poor to fair satisfaction scores, but a third achieved good to excellent result, with unchanged satisfaction in the long term. Reconstruction in a single stage using implants only or in combination with mastopexy was favoured in the lower grades, as opposed to a two-stage approach with TE followed by implant prosthesis in the higher grades. The fact that revisions were more common in the higher grades and unilateral deformities suggests that they are more difficult to manage, and that performing a two-stage reconstruction may be advantageous in achieving better symmetry, and enhancing patient satisfaction.
From this review, laterality and grades of deformity were important factors in the management of TBD. It is therefore essential to establish a treatment pathway that facilitates the correct planning and management of this complex deformity. Implementing the proposed algorithm in a perhaps larger study that includes evaluation criteria involving both the surgeon and patient may be an area worth exploring in the future.
Acknowledgments
The authors would like to thank all the plastic surgery consultants at Queen Elizabeth Hospital whom their patients were included in this review.
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/abs.2018.09.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The hospital clinical governance board and audit department approved this study. There were no ethical implications and therefore an ethical approval was not required.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- von Heimburg D, Exner K, Kruft S, et al. The tuberous breast deformity: classification and treatment. Br J Plast Surg 1996;49:339-45. [Crossref] [PubMed]
- Meara JG, Kolker A, Bartlett G, et al. Tuberous breast deformity: principles and practice. Ann Plast Surg 2000;45:607-11. [Crossref] [PubMed]
- Panchapakesan V, Brown MH. Management of tuberous breast deformity with anatomic cohesive silicone gel breast implants. Aesthetic Plast Surg 2009;33:49-53. [Crossref] [PubMed]
- Dessy LA, Mazzocchi M, Corrias F, et al. Correction of tuberous breast with small volume asymmetry by using a new adjustable implant. Eur Rev Med Pharmacol Sci 2013;17:977-83. [PubMed]
- Hsieh F, Shah A, Malata CM. Experience with the Mentor Contour Profile Becker-35 expandable implants in reconstructive breast surgery. J Plast Reconstr Aesthet Surg 2010;63:1124-30. [Crossref] [PubMed]
- Scuderi N, Alfano C, Campus GV, et al. Multicenter study on breast reconstruction outcome using Becker implants. Aesthetic Plast Surg 2011;35:66-72. [Crossref] [PubMed]
- Scheepers JH, Quaba AA. Tissue expansion in the treatment of tubular breast deformity. Br J Plast Surg 1992;45:529-32. [Crossref] [PubMed]
- Spear SL, Pelletiere CV, Menon N. One-stage augmentation combined with mastopexy: aesthetic results and patient satisfaction. Aesthetic Plast Surg 2004;28:259-67. [Crossref] [PubMed]
- Grolleau JL, Lanfrey E, Lavigne B, et al. Breast base anomalies: treatment strategy for tuberous breasts, minor deformities, and asymmetry. Plast Reconstr Surg 1999;104:2040-8. [Crossref] [PubMed]
- Persichetti P, Cagli B, Tenna S, et al. Decision making in the treatment of tuberous and tubular breasts: volume adjustment as a crucial stage in the surgical strategy. Aesthetic Plast Surg 2005;29:482-8. [Crossref] [PubMed]
Cite this article as: Salibi A, Thomas SS. An algorithm for the management of tuberous breast deformity. Ann Breast Surg 2018;2:17.