
Inferior mammary fold reconstruction in reconstructed breast: a novel technique
Introduction
The infra-mammary fold (IMF) is an important landmark in reconstructive breast surgery (1). When the IMF is violated in oncological mastectomy surgery, the reconstructed breast lacks a well-defined IMF, which is invariably lowered. Redefinition of the IMF restores the anatomical position of the IMF. This improves quality of life for the patient as it allows the breast to fit comfortably in a brassiere. It also defines the shape of the whole breast and contributes to the overall aesthetic appearance (2).
Many IMF reconstruction techniques have been previously described; both externally and internally in relation to the reconstructed breast. Pennisi (3) recreated the IMF externally under an implant-based breast reconstruction and Ryan (4) used a lower thoracic advancement flap to augment the lower pole of the reconstructed breast. The internal method introduced by Versaci (5) utilises the tissue expander (TE) capsule to reconstruct the IMF at the time of TE removal. Further modifications were described by Bogetti et al. (6) and Nava et al. (7) using the superficial fascia, which manages to overcome the bulkiness and scalloping of the IMF present in Versaci’s method. Despite all of the above, the internal methods still occasionally suffer from late loss of IMF definition in both implant-based and autologous reconstructed breast (8).
In this paper, an efficient surgical technique is described to restore the IMF in the reconstructed breast. This is mainly achieved post deep inferior epigastric perforator (DIEP) free flap reconstruction.
Methods
Surgical technique
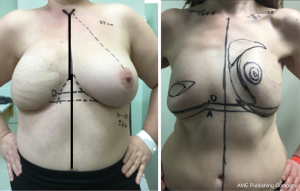
Pre-operatively, the inferior border of the reconstructed breast is identified and marked on the chest wall. The location of the new IMF is marked at 1 cm higher than the desired level. This is to allow for relaxation of the tissue during wound maturation. This demarcation is performed while the patient in standing position as shown in Figure 1.
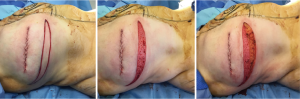
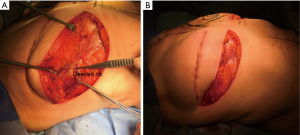
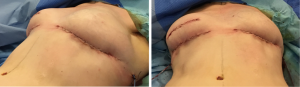
Intra-operatively, a crescent of skin, of about 2 cm in width at its widest and along the full length of the lower border of the reconstructed breast, is de-epithelialised accurately using a blade leaving healthy dermis, as shown in Figures 2,3. The lower edge of the remaining dermis is cut using monopolar diathermy down to the deep fascia over the pectoralis major muscle. Dissection is continued up under the breast on the chest wall to 1 cm above the desired new IMF level as shown in Figure 4A. The lower third of the reconstructed breast is raised, folded underneath, and the dermis is stitched to the periosteum of the ribs at the desired higher level using round-bodied 2/0 polydioxanone (PDS) interrupted sutures as shown in Figure 4B. Two rows of the PDS stitches are used to lay the dermis flat on the chest wall. This creates the hammock effect as seen in Figure 2B. The breast is adjusted so that it acquires reasonable projection and well-defined IMF. Dissection is performed inferiorly under the Scarpa’s fascia over the abdominal wall to allow advancement superiorly, as per reverse abdominoplasty, then secured to the same new IMF line using the same 2/0 PDS interrupted sutures that also passed through periosteum if possible as shown in Figure 2B,C. Finally, the skin edges are closed in layers using 3/0 monocryl suture as shown in Figure 5. A sub-cutaneous suction drain is left in the wound, which can be safely removed on day-2 postoperatively.
The periosteal sutures are very uncomfortable for the patient without local anaesthetic block for at least 5 days. The authors suggest the injection of local anaesthetic intra-operatively to block the intercostal nerves at the lower border of the ribs to which the breast lower edge is anchored. Alternatively, one can lay a pain buster catheter for infusion of local anaesthetic into the wound. This both controls the post-operative pain and shortens the recovery time.
Patients
This is a retrospective study of all cases that suffered from IMF loss following breast surgery and were reconstructed in our department using this original technique.
Results
All cases that needed IMF reconstruction were included in this study. There were nine patients in total during the period from January 2011 to April 2019. The average age of the patient was 49 years (range, 31–61 years). Two cases had IMF reconstruction following bilateral risk reducing skin-sparing mastectomy. One case required IMF revision following delayed DIEP reconstruction on one side and immediate DIEP on the other as seen in Figure 5. One case had the IMF reconstructed following bilateral delayed DIEP as shown in Figure 6. Two cases lost their IMF after unilateral DIEP reconstruction due to oncological mastectomy. Three cases had unilateral breast reconstruction using TE followed by implant and IMF reconstruction one of which had the IMF lowered rather than lifted up. All nine patients had IMF reconstruction using the same technique. The Follow up was one week post-operatively in the plastic dressing clinic followed by an out-patient appointment in 3 months’ time. All had a satisfactory outcome and no complications were recorded. Only two cases had mild surgical site erythema and inflammation that was treated conservatively with one-week course of oral antibiotics.

Discussion
Different surgical methods for recreating the IMF have been described throughout the years. Based on their access into the chest wall, they can be classified as: internal (5-9), external (3,4,10,11), or percutaneous (12,13). In the internal method, the surgeons attempt to restore the IMF from within the breast pocket, whereas in the external method the chest wall is accessed through a skin incision at the lower border of the breast.
In the percutaneous method, described by Hamdi et al. (12), the PDS suture is passed around the circumference of the breast then tunneled subcutaneously through multiple stab incisions at the IMF level to act as a purse-string stitch. While the percutanrous method described by Nakajima et al. (13), involved vertical pendulum polyglactin (VICRYL) sutures passed between pairs of small stab incisions along the desired IMF. Both techniques are used in implant-based reconstructed breast.
In this paper we are presenting an external approach. The disadvantage of this method, when compared to the other methods, might be the long extra scar at the lower border of the breast with risks of surgical site infection and wound breakdown. Additionally, the scar might not be of a high aesthetic value from a cosmetic perspective. In spite of all this, it is a robust technique that utilises autologous strong tissue - the designed dermis - to support the lower edge of the reconstructed breast, improve its contour and projection and more importantly allows the breast to fit comfortably in a brassiere.
In summary this technique is easy to perform, reliable, and reproducible. It can be used in autologous and implant-based reconstructed breast. The key is in the execution of pre-operative markings.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/abs.2019.10.04). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). This study has been approved by the ethical committee in Salisbury NHS Foundation Trust. All patients included in the study are consented for their data and photographs to be used for research and publications.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Carlson GW, Grossl N, Lewis MM, et al. Preservation of the inframammary fold: what are we leaving behind? Plast Reconstr Surg 1996;98:447-50. [Crossref] [PubMed]
- Maclin MM 2nd, Deigni OA, Bengtson BP. The Laminated Nature of the Pectoralis Major Muscle and the Redefinition of the Inframammary Fold: Clinical Implications in Aesthetic and Reconstructive Breast Surgery. Clin Plast Surg 2015;42:465-79. [Crossref] [PubMed]
- Pennisi VR. Making a definite inframammary fold under a reconstructed breast. Plast Reconstr Surg 1977;60:523-5. [Crossref] [PubMed]
- Ryan JJ. A lower thoracic advancement flap in breast reconstruction after mastectomy. Plast Reconstr Surg 1982;70:153-60. [Crossref] [PubMed]
- Versaci AD. A method of reconstructing a pendulous breast utilizing the tissue expander. Plast Reconstr Surg 1987;80:387-95. [Crossref] [PubMed]
- Bogetti P, Cravero L, Spagnoli G, et al. Aesthetic role of the surgically rebuilt inframammary fold for implant-based breast reconstruction after mastectomy. J Plast Reconstr Aesthet Surg 2007;60:1225-32. [Crossref] [PubMed]
- Nava M, Quattrone P, Riggio E. Focus on the breast fascial system: a new approach for inframammary fold reconstruction. Plast Reconstr Surg 1998;102:1034-45. [Crossref] [PubMed]
- Tomita K, Yano K, Nishibayashi A, et al. Aesthetic outcomes of inframammary fold recreation in two-stage, implant-based, breast reconstruction. Springerplus 2016;5:1656. [Crossref] [PubMed]
- Persichetti P, Langella M, Filoni A, et al. How to redefine the inframammary fold: the "slingshot" capsular flap. Ann Plast Surg 2013;70:636-8. [Crossref] [PubMed]
- Atiyeh B, Ibrahim A, Saba S, et al. The Inframammary Fold (IMF): A Poorly Appreciated Landmark in Prosthetic/Alloplastic Breast Aesthetic and Reconstructive Surgery-Personal Experience. Aesthetic Plast Surg 2017;41:806-14. [Crossref] [PubMed]
- Campbell CF, Small KH, Adams WP Jr. The Inframammary Fold (IMF) Fixation Suture: Proactive Control of the IMF in Primary Breast Augmentation. Aesthet Surg J 2016;36:619-23. [Crossref] [PubMed]
- Hamdi M, Anzarut A, Hendrickx B, et al. Percutaneous Purse-String Suture: An Innovative Percutaneous Technique for Inframammary Fold Creation and Improved Breast Projection in Reconstructive Surgery. Aesthet Surg J 2018;38:1298-303. [Crossref] [PubMed]
- Nakajima Y, Kondoh S, Nishioka H, et al. A new percutaneous method for inframammary fold reconstruction in implant-based breast reconstruction: Vertical pendulum suture. Medicine (Baltimore) 2018;97:e11964 [Crossref] [PubMed]
Cite this article as: Hijazi Y, Brewin M, McGuiness C. Inferior mammary fold reconstruction in reconstructed breast: a novel technique. Ann Breast Surg 2019;3:26.


