
Incisional negative pressure wound therapy on mastectomy skin flaps—does it reduce seroma formation? A prospective, randomized study
Introduction
Breast cancer is affecting one in 10 women, and is the most common cancer in women in the Western world. In Denmark, approximately 4,000 women are diagnosed with breast cancer every year. Breast conserving surgery is the most common procedure and one fourth of women with breast cancer undergo radical mastectomy (1-3).
The most frequent complication to mastectomy is formation of seroma, affecting nearly all mastectomised women. Seroma is a pool of serous fluid in the mastectomy cavity. It is formed in the acute postsurgical phase due to (I) an acute inflammatory response to the surgical trauma and/or (II) by leaking from the lymph vessels disrupted during sentinel lymph node biopsy or axillary clearance procedure. If not drained the accumulation of seroma distends the wound cavity leading to increased risk of delayed wound healing, wound dehiscence, necrosis of skin flaps and surgical site infection. Drainage is therefore necessary multiple times through weeks postoperatively. For newly operated women, this results in several demanding outpatient’s visits. The drainages cost increased risk of iatrogenic infection (2,4-12).
The majority of women treated for breast cancer need postsurgical adjuvant therapy. Complications to surgery are not only stressful and giving physical discomfort but also delays onset of the adjuvant treatment possibly affecting the oncologic safety and increased cost to the health system (12-15).
Among other methods, mastectomy cavity- and axillary paddings, reduce seroma formation. The technique involves closing dead space by suturing the fascia with regional muscles (16).
Incisional negative pressure wound therapy (iNPWT) is when a mechanical device connected to a dressing applies negative pressure on the underlying closed incision. Biomechanical studies have shown that iNPWT leads to removal of interstitial fluid, increases oxygen saturation, angiogenesis and increases blood and lymph flow. This has demonstrated beneficial effect on wound healing and reduces risk of infection, wound dehiscence, haematoma/seroma formation, incisional drainage and lymphedema in the surgical site (3,17-19).
In 2017, Willy et al. published an international multidisciplinary consensus recommendations article of closed incision negative pressure therapy. They recommended iNPWT in patients with a surgical incision that is historically at high risk for developing surgical site complications. Furthermore, iNPWT is recommended for patients with one or more comorbidity such as diabetes mellitus, advanced age, obesity (BMI ≥30 kg/m2), tobacco use, hypoalbuminaemia and corticosteroid use (14).
A reduction in seroma formation has been studied. Effect on seroma formation after mastectomy is, however, unknown (3,14,20-23).
The purpose of this study was to investigate the potential effect of iNPWT on seroma formation in women undergoing mastectomy with sentinel lymph node biopsy and mastectomy with axillary clearance.
Methods
We conducted a randomized controlled trial to investigate if iNPWT reduced seroma formation compared to standard dressing in mastectomised women. Two different procedures were studied: (I) women having mastectomy and sentinel lymph node biopsy and (II) women having mastectomy and axillary clearance. Women were randomly assigned to iNPWT (intervention) or a standard postoperative dressing (control group). The study was unblinded. For iNPWT we used PICO Negative Pressure Wound Therapy of 20 cm × 20 cm (7.9×7.9 in.) delivering a negative pressure of 80 mmHg (Smith & Nephew, Hull, UK).
The control group patients were randomized to a non-compressive, breathable 3M Micropore Surgical Paper Tape.
The primary endpoint was total amount of seroma formation by aspiration procedure (measured in mL) and the secondary endpoints were number of drainage days and postoperative complications (i.e., surgical site infection, necrosis, wound dehiscence).
Sample size
Based on the results from two previous studies (Pachowsky, Pauser) we estimated that prophylactic use of iNPWT could reduce the amount of seroma formation with 50% compared to standard dressings. Based on this hypothesis we determined that obtaining power of 0.80 and a significance level of 0.05 when assuming seroma production between 50 and 1,636 mL, would result in need for a total of 36 patients in the sentinel lymph node biopsy group (18 intervention, 18 controls). Similarly, assuming a seroma production between 380 and 1,470 mL, a total of 30 patients would be needed in the axillary clearance group.
Participants
Eligible participants were women treated for breast cancer or ductal carcinoma in situ with a mastectomy at Odense University Hospital during 2015–2018. The women were recruited by one of four doctors at the first visit to the Department of Plastic and reconstructive surgery. The women were given both oral and written information on the project and a folder of their legal rights at the pre-surgical information. It was extensively described to the women that they at any time could leave the study if they wished without affecting their further treatment. The women were enrolled when written consent was given at a later follow-up by a nurse.
Patients mastectomised due to ipsilateral breast cancer recurrence, after neo adjuvant chemotherapy, with inflammatory breast cancer or with cutaneous involvement were not included.
Only women speaking Danish and not suffering from dementia or psychiatric disorders were included.
Intervention
The mastectomy was initiated with sentinel lymph node biopsy procedure if no pre-surgical histologic verified axillary lymph node metastasis was known. During this procedure, typically 1–3 lymph nodes were identified and removed. Afterwards the breast tissue was removed leaving only enough skin to ensure closure without extensive stretch. Both axillary lymph node dissection and sentinel lymph node biopsy is done through the mastectomy incision.
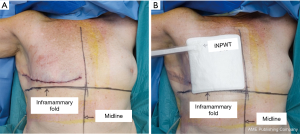
At this point randomization was done. At the end of the procedure a drain was placed from the surgical cavity through the subcutis and the skin lateral and distal from the wound. It was placed in a manner to allow the iNPWT to cover the mastectomy cavity (Figure 1). The skin was then closed using absorbable monofilament sutures and covered with either iNPWT (PICO bandage 20 cm × 20 cm (7.9×7.9 in.) delivering a negative pressure of 80 mmHg (Smith & Nephew, Hull, UK) or standard dressing (MicroporeTM tape, 3 M, Copenhagen, Denmark). The drain was removed the following day and the women discharged from the hospital.
If axillary lymph node involvement was known pre-operatively or the perioperative histologic examination of the sentinel lymph nodes showed metastasis the procedure was done as the above explained mastectomy followed by an axillary clearance. An axillary clearance comprises removal of all lymph nodes and adipose tissue in the triangular region of the axilla including level I and II.
Both the iNPWT and the Micropore were left in situ for 7 days.
Randomization
We used a 1:1 randomization list of the two patients’ strata: (I) mastectomy and sentinel lymph node biopsy (n=19 intervention and n=19 controls) and (II) mastectomy and axillary clearance (n=14 intervention and n=14 controls). On the randomization list a specific number and letter code was linked to the patient number. We made randomization envelopes containing the specific number and letter code (Fx.GD4) and either “Intervention” or “Control”. After surgery the randomization was performed by the nurse in the operating theatre opening the next envelope in the randomization box either Intervention (iNPWT) or Control (Micropore) bandage.
Ethics, approval and data management
The Regional Scientific Ethical Committee of Southern Denmark (S-20150052) and the Danish Data Protection Agency (18/22685) approved the study. The data were stored on a secure server at Region of Southern Denmark.
Data collection, outcomes and statistical analysis
All women were seen at clinical visits by a nurse at the department of breast surgery day 3, 5, 7, 10, 13, 16 and 19 after surgery. At these check-ups the nurse aspirated seroma from the surgical site independent of clinical recognized amount of seroma. The amounts of seroma aspirated was noted in the files as well as any postoperative complications (infection, dehiscence or skin necrosis).
The primary outcome in this study was cumulative volume of aspirated seroma. Secondary outcomes were cumulative number of aspirations and complications as hematoma, necrosis, dehiscence and surgical site infection registered up to 30 days postsurgical. Furthermore, data on possible confounders as age, Body Mass Index, breast specimen weight, number of lymph nodes removed, number of involved lymph nodes, smoking and co-morbidities were assessed prospectively through manual examination of the medical records.
We reported baseline characteristics by counts and proportions for categorical variables and means with standard deviation for numerical variables.
Moreover, we compared baseline characteristics between iNPWT bandage and conventional wound dressing. All analysis was done for both the sentinel lymph node biopsy group and for the axillary clearance group separately. We used Fisher’s exact test for categorical variables, t-test for normally distributed and Wilcoxon rank sum test for non-normally distributed, depending on the normal distribution of the variables assessed by Shapiro-Wilk’s test. Furthermore, we in a supplementary analysis applied linear regression to investigate association between seroma production and bandage adjusting for patient characteristics. If the participants had their iNPWT removed due to complication or malfunction during the follow-up they were excluded from the analysis.
Results
Trial participants
A total of 66 women were included in the study. The sentinel lymph node biopsy group consisted of 19 iNPWTs and 19 controls (EXPECTED 18+18) and the mastectomy and axillary clearance consisted of 14 iNPWTs and 14 controls (EXPECTED 15+15). The last patient was enrolled in November 2017 and follow-up was concluded January 2018. Baseline characteristics and perioperative patient characteristics is shown in Table 1. It is seen that these are similar for intervention and controls in the axillary clearance group but differ regarding age and smoking in the sentinel lymph node biopsy group. In the sentinel lymph node biopsy group, however, mean age was 7 years higher in the control group and smoking significant higher in the iNPWT group. Body Mass Index and weight of breast was comparable.
Table 1
| Variables | Mastectomy and sentinel lymph node biopsy* | Mastectomy and axillary clearance* | |||||
|---|---|---|---|---|---|---|---|
| SPD | iNPWT | P value | SPD | iNPWT | P value | ||
| Number of patients | 19 | 19 | 14 | 14 | |||
| Age [mean (SD)] | 71 (7.5) | 64 (12.0) | 0.038 | 65 (11.5) | 65 (12.9) | 0.854 | |
| Body mass index [mean (SD)] | 26.9 (3.9) | 25.6 (4.0) | 0.303 | 25.3 (3.5) | 27.2 (5.1) | 0.263 | |
| Weight of breast [mean (SD)] | 834 (301) | 991 (260) | 0.064 | 761 (356) | 766 (497) | 0.977 | |
| Number of lymph nodes (mean) | 5.5 (7.6) | 5.2 (6.4) | 0.383 | 13.8 (7.8) | 15.9 (9.7) | 0.565 | |
| Smoking | 1 (5%) | 7 (37%) | 0.042 | 3 (21%) | 3 (21%) | 1.000 | |
| Number of comorbidities [mean (SD)] | 1.11 (1.15) | 0.89 (1.10) | 0.505 | 1.21 (1.25) | 1.43 (1.09) | 0.401 | |
*The women are grouped into a sentinel lymph node biopsy and an axillary clearance group.
The overall age of the trial participants ranged from 37 to 81 years mean (66). Body mass index ranged from 18 to 40 with an overall mean BMI of 26. Breast weight ranged from 127 to 1,524 gram with an overall mean of 754 g.
The average number of lymph nodes resected was 5 (5.2–5.7) and 14 (13.8–15.9) for the sentinel lymph node group and the axillary clearance group, respectively (Table 1).
Number of women with comorbidities, such as heart and lung diseases, was few and equally distributed in Strada and randomization groups.
Primary outcome
The amount of seroma aspirated and number of aspirations is shown for each subgroup in Table 2. In the sentinel lymph node biopsy group, we found a mean volume of aspirated seroma of 320 and 457 mL in the iNPWT and control group respectively (P=0.140).
Table 2
| Variables | Mastectomy and sentinel lymph node biopsy* | Mastectomy and axillary clearance* | |||||
|---|---|---|---|---|---|---|---|
| SPD | iNPWT | P value | SPD | iNPWT | P value | ||
| Number of patients | 19 | 19 | 14 | 14 | |||
| Primary outcomes | |||||||
| Amount of seroma, ml aspirated [mean (min./max.)] | 457 (45/1,400) | 320 (15/787) | 0.140 | 767 (60/1,665) | 1103 (171/4,510) | 0.505 | |
| Secondary outcomes | |||||||
| Seroma aspiration days [mean (min./max.)] | 5 (2/8) | 4 (1/7) | 0.095 | 6 (2/7) | 7 (4/15) | 0.423 | |
| Infection | 1 | 3 | |||||
| Skin necrosis | 1 | 1 | |||||
*, the women are grouped into a sentinel lymph node biopsy and an axillary clearance group. SPD, standard postoperative dressing; iNPWT, incisional negative pressure wound therapy.
In the axillary clearance group, we found a slightly higher volume of aspirated seroma in the iNPWT group (1,103 mL) compared to the control group (767 mL) (P=0.505).
Secondary outcome
Number of infections and skin necrosis within 30 days of surgery is shown in Table 2. Individual patient characteristics are shown in Table 3. A total of 4 patients (6.2%) were treated for infection with antibiotics without surgical intervention. The four patients were distributed with one patient in the control sentinel lymph node biopsy group and three patients in the intervention axillary clearance group. Superficial, minor necrosis was seen in 2 cases (3.1%); distributed with one case patient in the intervention axillary clearance group and one patient in the control sentinel node group. A revision in local and general anesthesia was performed.
Table 3
| No. | Patient sub group | Age | Comorbidity | Smoker | Breast weight/seroma volume/emptying days | Complication | |
|---|---|---|---|---|---|---|---|
| 1 | SN | Control | 68 | DM, HA, BMI 30 | Yes | 1,243 gr/300 mL/4 days | Infection |
| 2 | AXIL | Intervention | 63 | BMI 27 | Yes | 660 gr/1,115 mL/9 days | Infection |
| 3 | AXIL | Intervention | 82 | HA, BMI 27 | Yes | 604 gr/505 mL/5days | Infection |
| 4 | AXIL | Intervention | 67 | COL, BMI 18 | Yes | 127 gr/830 mL/8 days | Infection |
| 5 | SN | Control | 62 | BMI 30 | No | 906 gr/400 mL/6 days | Superficial necrosis |
| 6 | AXIL | Intervention | 69 | HA, BMI 30 | No | 845 gr/755 mL/7 days | Superficial necrosis |
Complications within 30 days postoperative to either mastectomy and sentinel lymph node biopsy and axillary clearance. SN, Sentinel lymph node group; AXIL, axillary clearance group; HA, hypertensio arterialis; DM, diabetes mellitus; COL, chronic obstructive lung disease; BMI, body mass index.
The 6 patients having postoperative complications were 60 years of age or older at the time of surgery. In 4 out of the 6 cases the patient subgroup was mastectomy and axillary clearance. We found no cases of wound ruptures.
A strong association between Body Mass index and breast weight with total aspirated seroma volume was found. An increase in breast specimen weight of 100 g resulted in an increase in aspirated volume of 47 mL (P=0.002) and 138 mL (P<0.001) in the sentinel lymph node biopsy group and the axillary clearance group, respectively, when adjusting for wound dressing.
The amount of seroma drainage days in the sentinel lymph node biopsy group was 5 in the control group and 4 days in the iNPWT group (P=0.095). In the axillary clearance group, it was 6 and 7 days (P=0.423), respectively.
Discussion
Main findings
The study did not demonstrate a significant effect of 7 days of iNPWT in reducing seroma and postoperative complications following mastectomy and sentinel lymph node biopsy or mastectomy and axillary clearance.
A slight tendency toward a reduction in seroma formation and number of aspirations with the use of iNPWT was found in the mastectomy and sentinel lymph node biopsy group.
Other studies and interpretations
To our knowledge only few other studies have investigated a possible association of iNPWT and seroma formation after breast surgery.
Ferrando et al. (24) included 37 women undergoing a variety of oncologic breast surgery procedures. Some had simple mastectomy or breast conserving surgery while other had skin sparing mastectomy followed by 1- or 2-stage implant reconstruction or reconstruction with autologous flap. The participants were not randomized but simply chose iNPWT or standard postsurgical dressing. No information regarding lymph node removal was given. They reported reduced postsurgical complications in general in the iNPWT vs. standard dressing group. They did, however, not measure seroma volume nor explain the regimen of drains used. Several randomized studies on orthopedic surgical procedures have been published.
Nordmeyer et al. (21) randomized 20 patients undergoing surgical treatment for spinal fracture to either iNPWT (PICO) or standard postsurgical dressing. They found that iNPWT was highly associated with decreased seroma formation. Pachowsky et al. (22) randomized 19 patients undergoing hip arthroplasty to either iNPWT (Prevena) or standard postsurgical dressing and found a significant reduction of postsurgical seroma using an iNPWT compared to conventional wound dressing (P<0.021) The average size of seroma in the control and the case group was respectively 5.08 and 1.07 mL. Likewise, Pauser et al. (25) described significant reduction of postoperative seroma using an iNPWT (Prevena) compared to conventional wound dressing (P<0.05) following a hemiarthroplasty for femoral neck fractures. The seroma formation was measured by ultrasound in the Pachowsky and Pauser study. The significant reduction of seroma formation in these two studies is based on very small volumina.
A randomized controlled study (Hyun-Suk et al.) (26) from Department of Plastic Reconstructive Surgery, Republic of Korea, was published in 2016. They included 100 patients after Superficial Circumflex Iliac Artery Perforator Flap Harvest and found significant earlier removal of suction drains when placing an iNPWT (CuraVAC) on the closed incision lines compared to conventional wound dressing (P=0.0004 and P=0.077).
The four studies mentioned above examine a surgical site with minimal seroma formation as compared to the seroma formation in mastectomy patients with added lymph node procedures.
It is well known that a mastectomy procedure leads to a large surgical cavity and as with other mastectomy cavities a high risk of seroma formation. Adding axillary clearance with disruption of all lymph vessels in level I and II imply severely increased seroma formation. Removing only a few sentinel lymph nodes will also increase the seroma formation although not to an extent as with axillary clearance (4,5,12).
It might be possible that iNPWT reduces seroma from surgical cavities but not from disrupted lymph vessels. The tendency toward reduction in seroma formation found in our sentinel lymph node biopsy could then be explained by a reduction in seroma formation from the mastectomy cavity due to iNPWT but blurred by seroma formation from the sentinel lymph node biopsy. If this were the case the reducing effect of iNPWT would be overshadowed completely in the axillary clearance group.
Angspatt et al. (27) studied iNPWT (Renasys, Smith and Nephew, Oklahoma, USA) in Latissimus Dorsi Flap donor site. This donor site defect resembles the cavity after simply mastectomy without lymph node procedures. Among 40 women treated with either iNPWT or standard dressing both aspirated volume and number of aspirations were significantly reduced in the iNPWT group.
Strength and limitations
Our groups to compare in the sentinel lymph node group differed regarding both age and smoking. Nevertheless, none of these seemed in the regression analysis to be correlated with seroma formation and confounding is probably minimal.
A limitation of our study is that we used an iNPWT only covering the mastectomy skin flaps and not the axillary area. This was chosen because we wanted the dressing to be quick and easily applicable. If the dressing was to cover both the axilla and the mastectomy area minimum two iNPWT had to be used increasing surgery time. Additionally, we expected difficulties in achieving a well-functioning close dressing for minimum 7 days in the axilla. Any effect of iNPWT can therefore be ascribed to the effect of iNPWT on the mastectomy cavity. It seemed that seroma from the axilla is severely larger than we expected and thereby blurring the results. Simply mastectomy without axillary procedure (clearance or lymph node biopsy) is seldom and therefore not as clinical relevant to study as mastectomy with any axillary procedure.
In the initial hypothesis of reducing the seroma formation with 50% the power calculation stated the number of participants to respectively; (n=18 controls and n=18 cases) in the seroma group and (n=15 controls and n=15 cases) in the axillary dissection group. We included a total of 66 participants. An effect of 50% might have been optimistic in this patient group, especially in the axillary clearance group, but this was made on the published data at that time. This study therefore failed to show clear effect on the seroma formation due to few numbers, but might, hopefully, add cases to the literature and future evidence. Seroma reduction is, however, only one criteria of surgical morbidity.
The nurses in charge of the check-ups are highly experienced in the seroma aspiration procedure. They are always evaluating whether the volume is high enough for aspiration. Variability in clinical amount of seroma leading to aspiration cannot be avoided.
The economic costs of treatment with the iNPWT must be taken into account when discussing the strength and limitations of this study. The iNPWT bandage is substantially more expensive than the conventional dressing method, Micropore plaster. We did not include cost effectiveness analysis of the INWPT on seroma formation in this paper. The dressing has, however, previously been shown to be cost-effective due to decreased risk of infections in cesarean sections in a high-risk population (23). A large proportion of the mastectomised women need further adjuvant therapy. Avoiding infections and delay of adjuvant therapy is extremely important in order to achieve most optimal oncologic treatment.
A possible effect on seroma formation using a more expensive bandage might be cost-effective if a reduction in drainage, seroma induced complications and shorter hospitalization can be seen.
Conclusions
This study tested if iNPWT on the mastectomy skin flaps reduces seroma in women undergoing mastectomy and sentinel lymph node biopsy and women undergoing mastectomy and axillary clearance. The effect of iNPWT was probably blurred by seroma from the axilla and the study failed to show a substantially effect of iNPWT on the mastectomy flaps alone, counterbalancing the financial expense and additional difficulties associated with applying and wearing the iNPWT.
Acknowledgments
Funding: The PICO bandages were funded by Smith & Nephew. There are no other economical expenses in the project. The participants are covered by the patient insurance scheme and the sponsor-investigator is covered by the hospital’s mandatory insurance.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/abs.2020.01.01). CB serves as an unpaid editorial board member of Annals of Breast Surgery from Aug 2019 to Jul 2021. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The Regional Scientific Ethical Committee of Southern Denmark (S-20150052) and the Danish Data Protection Agency (18/22685) approved the study. The data were stored on a secure server at Region of Southern Denmark. The women were given both oral and written information on the project and a folder of their legal rights at the pre-surgical information.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
-
Kvalitetsindikatorrapport for Brystkræft 2012 . Available online: www.dbcg.dk/PDF%20Filer/DBCG_rapport_2012.pdf - Ghoncheh M, Pournamdar Z, Salehiniya H. Incidence and Mortality and Epidemiology of Breast Cancer in the World. Asian Pac J Cancer Prev 2016;17:43-6. [Crossref] [PubMed]
- Strugala V, Martin R. Meta-Analysis of Comparative Trials Evaluating a Prophylactic Single-Use Negative Pressure Wound Therapy System for the Prevention of Surgical Site Complications. Surg Infect (Larchmt) 2017;18:810-9. [Crossref] [PubMed]
- Mazouni C, Mesnard C, Cloutier AS, et al. Quilting Sutures Reduces Seroma in Mastectomy. Clin Breast Cancer 2015;15:289-93. [Crossref] [PubMed]
- Srivastava V, Basu S, Shukla VK. Seroma Formation after Breast Cancer Surgery: What We Have Learned in the Last Two Decades. J Breast Cancer 2012;15:373-80. [Crossref] [PubMed]
- Iovino F, Auriemma PP, Ferraraccio F, et al. Preventing seroma formation after axillary dissection for breast cancer: a randomized trial. Am J Surg 2012;203:708-14. [Crossref] [PubMed]
- van Bemmel AJ, van de Velde CJ, Schmitz RF, et al. Prevention of seroma formation after axillary dissection in breast cancer: a systematic review. Eur J Surg Oncol 2011;37:829-35. [Crossref] [PubMed]
- Turner EJ, Benson JR, Winters ZE. Techniques in the prevention and management of seromas after breast surgery. Future Oncol 2014;10:1049-63. [Crossref] [PubMed]
- ten Wolde B, van den Wildenberg FJ, Keemers-Gels ME, et al. Quilting prevents seroma formation following breast cancer surgery: closing the dead space by quilting prevents seroma following axillary lymph node dissection and mastectomy. Ann Surg Oncol 2014;21:802-7. [Crossref] [PubMed]
- Zieliński J, Jaworski R, Irga N, et al. Analysis of selected factors influencing seroma formation in breast cancer patients undergoing mastectomy. Arch Med Sci 2013;9:86-92. [Crossref] [PubMed]
- Coveney EC, O'Dwyer PJ, Geraghty JG, et al. Effect of closing dead space on seroma formation after mastectomy: a prospective randomized clinical trial. Eur J Surg Oncol 1993;19:143-6. [PubMed]
- Turner EJ, Benson JR, Winters ZE. Techniques in the prevention and management of seromas after breast surgery. Future Oncol 2014;10:1049-63. [Crossref] [PubMed]
- Holt R, Murphy J. PICO™ incision closure in oncoplastic breast surgery: a case series. Br J Hosp Med (Lond) 2015;76:217-23. [Crossref] [PubMed]
- Willy C, Agarwal A, Andersen CA, et al. Closed incision negative pressure therapy: international multidisciplinary consensus recommendations. Int Wound J 2017;14:385-98. [Crossref] [PubMed]
- Matusiak D, Wichtowski M, Pieszko K, et al. Is negative-pressure wound therapy beneficial in modern-day breast surgery? Contemp Oncol (Pozn) 2019;23:69-73. [Crossref] [PubMed]
- Garbay JR, Thoury A, Moinon E, et al. Axillary Padding without Drainage after Axillary Lymphadenectomy - a Prospective Study of 299 Patients with Early Breast Cancer. Breast Care (Basel) 2012;7:231-5. [Crossref] [PubMed]
- Available online: www.smith-nephew.com/PICOMIB
- Nagata T, Miura K, Homma Y, et al. Comparison between Negative-Pressure Fixation and Film Dressing in Wound Management after Tissue Expansion: A randomized Controlled Trial. Plast Reconstr Surg 2018;142:37-41. [Crossref] [PubMed]
- Kim DY, Park SJ, Bang SI, et al. Does the Use of Incisional Negative-Pressure Wound Therapy Prevent Mastectomy Flap Necrosis in Immediate Expander-Based Breast Reconstruction? Plast Reconstr Surg 2016;138:558-66. [Crossref] [PubMed]
- Closed surgical incision management: Understanding the role of NPWT. Available online: www.wuwhs2016.com/files/WUWHS_SI_consensus_Web.pdf
- Nordmeyer M, Pauser J, Biber R, et al. Negative Pressure Wound Therapy for seroma prevention and surgical incision treatment in spinal fracture care. Int Wound J 2016;13:1176-9. [Crossref] [PubMed]
- Pachowsky M, Gusinde J, Klein A, et al. Negative pressure wound therapy to prevent seromas and treat surgical incisions after total hip arthroplasty. Int Orthop 2012;36:719-22. [Crossref] [PubMed]
- Hyldig N, Vinter CA, Kruse M, et al. Prophylactic incisional negative pressure wound therapy reduces the risk of surgical site infection after caesarean section in obese women: a pragmatic randomised clinical trial. BJOG 2019;126:628-35. [Crossref] [PubMed]
- Ferrando PM, Ala A, Bussone R, et al. Closed Incision Negative Pressure Therapy in Oncological Breast Surgery: Comparison with Standard Care Dressings. Plast Reconstr Surg Glob Open 2018;6:e1732 [Crossref] [PubMed]
- Pauser J, Nordmeyer M, Biber R, et al. Incisional negative pressure wound therapy after hemiarthroplasty for femoral neck fractures – reduction of wound complications. Int Wound J 2016;13:663-7. [Crossref] [PubMed]
- Peter Suh HS, Hong JP. Effects of Incisional Negative Wound Pressure therapy on Primary Closed Defects after Superficial Circumflex Iliac Perforator Flap Harvest. Plast Reconstr Surg 2016;138:1333-40. [Crossref] [PubMed]
- Angspatt A, Laopiyasakul T, Pungrasmi P, et al. The Role of Negative-Pressure Wound Therapy in Latissimus Dorsi Flap Donor Site Seroma Prevention: A Cohort Study. Arch Plast Surg 2017;44:308-312. [Crossref] [PubMed]
Cite this article as: Larsen AK, Hyldig N, Möller S, Bille C. Incisional negative pressure wound therapy on mastectomy skin flaps—does it reduce seroma formation? A prospective, randomized study. Ann Breast Surg 2020;4:5.

