
Multicentric breast cancer comprising of three different histopathological types: a case report
Introduction
Breast cancers are defined as multicentric when it originates from different duct collecting systems with two or more synchronous ipsilateral neoplasms, separated by benign tissue located within different quadrant of the breast (1). The incidence of unilateral multiple breast cancer has been reported to account for approximately 5% of all breast cancers (2). We, herein, report a rare case of a post-menopausal lady with a unilateral multicentric breast cancer comprising of three different histopathological types. We present the following article in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/abs-19-101).
Case presentation
A 57-year-old lady presented with a left breast lump for 1 year. The lump was progressively increasing in size and there was no associated nipple discharge. She attained menarche at the age of 15 years old and menopause at the age of 52. She is married and blessed with 4 children. There was neither history of taking oral contraceptives nor any hormone replacement therapy. She denies smoking and alcohol intake. There was no family history of breast cancer or other malignancies in her family.
Physical examination demonstrated a lobulated swelling of the left breast with multiple satellite nodules and erythematous skin changes. The swelling was mobile, hard in consistency and the nipple was distorted. Multiple mobile left axillary lymph nodes were palpable. The right breast was normal and there were no signs of metastases.
A bilateral breast ultrasound demonstrated a large lobulated mass at the left lower region extending to the sub areolar with small nodules adjacent to the mass. There was also extensive edema with multiple lymphadenopathies at left axillary region.
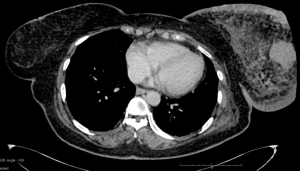
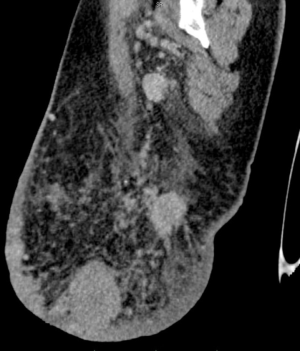
Subsequently, contrast enhanced computed tomography (CECT) (Figures 1,2) showed multicentric left breast lesion, most likely breast carcinoma with regional axillary lymph nodes involvement. Histopathological examination of a core biopsy over the left breast lesion revealed an invasive carcinoma. Clinical staging was T4bN1M0.
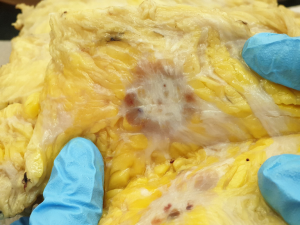
The patient underwent six cycles of neo-adjuvant chemotherapy, FEC regime (5-fluorouracil, epirubicin, cyclophosphamide), followed by mastectomy and axillary dissection after its completion. Histopathological examination of mastectomy specimen showed mixed mucinous carcinoma (mucinous component 40%), invasive ductal carcinoma (40%) and carcinoma with neuroendocrine features (20%) (Figures 3-5).

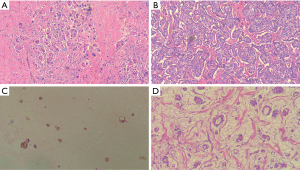
Morphologically, the largest breast lesion [upper outer quadrant (UOQ)] showed malignant cells in interconnecting sheets, trabeculae and cords (Figure 5A) with 15% glandular formation. In less than 30% of the areas, mucinous extravasation was noted. The malignant cells were moderate to markedly pleomorphic and have vesicular nuclei. There were occasional prominent nucleoli and moderate amount of cytoplasm. Signet ring cells were also noted. Mitosis was 1 in 10 high power fields.
The second largest breast lesion [upper inner quadrant (UIQ)] showed interconnecting sheets of malignant cells (Figure 5B) with very minimal glandular formation. The malignant cells were mild to moderately pleomorphic and have hyperchromatic nuclei, inconspicuous nucleoli and moderate amount of granular cytoplasm. Occasional bizarre malignant cells were also noted. They were positive toward synaptophysin+ (Figure 5C) but negative for chromogranin–. Mitosis was absent.
The smallest breast lesion [lower inner quadrant (LIQ)] showed extensive mucinous extravasation with floating malignant cells in small nest and trabeculae (Figure 5D). The malignant cells were moderate to markedly pleomorphic and have vesicular nuclei and prominent nucleoli and moderate amount of cytoplasm. Overall, the stroma was fibrotic. Lymphovascular invasion and dermal lymphovascular were present. Ductal carcinoma in situ (DCIS) of high nuclear grade, usual ductal hyperplasia and benign ductal papilloma were also noted. No Paget’s disease of the nipple or direct skin involvement was identified. The malignant tumor involved at superior margin. In total, 21 reactive lymph nodes were examined. Nineteen out of these lymph nodes were involved by malignant cells. Extranodal extension was also present. The malignant tumors expressed estrogen receptor and progesterone receptor protein. Her2 protein expression was negative. Diagnosis of mucinous carcinoma, carcinoma with neuroendocrine feature and mixed mucinous carcinoma (mucinous type and no special type) with modified Bloom and Richardson grade 2 (score 6–7) was given.
Later, whole body bone scan however showed increased tracer uptake in the left parietal bone, right shoulder, left sternoclavicular joint, left 2nd rib (anterior), left 3rd rib (posterior), T11 vertebra, L4/L5 vertebrae, left ischium, sacroiliac joints, and sacrum is due HDP-avid skeletal metastasis. She was then referred to Oncologist for further management unfortunately refused for further treatment.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Discussion
Breast cancer with multiple simultaneous foci has been a well-known issue for decades (2). When there is more than one distinct tumor within the same quadrant of the breast it is defined as multifocal and when multiple cancers develop in different quadrants of the breast it is defined as multicentric (3).
The diagnosis of unilateral multifocal breast cancer is usually made following a detailed histological examination of the dissected specimens. CECT (4) and magnetic resonance imaging (MRI) (5) have been reported to reveal a unilateral multiple breast cancer prior to surgery. Similarly demonstrated in our patient where preoperative CECT showed multicentric left breast lesion.
Based on recent studies, surgical options on multicentric or multifocal breast cancer (MMBC) women may undergo breast-conserving surgery as long as the principles of negative margins, appropriate radiotherapy and acceptable cosmesis are met (6-9). Most of them reported a loco-regional recurrence range of 3.0% to 5.1% at a 6-year follow-up in MMBC women with breast conservation, and there was no difference from the patients with unifocal tumor. Furthermore, they did not find any apparent differences in terms of disease-free survival or cosmetic result between MMBC patients and women with unifocal breast cancer after breast-conserving treatment. Hence, breast-conserving surgery is an option and effective for MMBC patients. Another study concluded that breast conserving surgery was a safe option in selected MMBC cases, particularly those women aged 50–69 years old with small multifocal tumor (<1 cm) and without an extensive DCIS component (10).
Multicentric breast cancers have a negative impact on prognosis. They are related to higher loco-regional and distant relapse independently from the type of surgery performed. Multicentric tumors have a worse biological behavior and that the presence of multiple foci should be considered in planning adjuvant treatments (11).
Conclusions
Multicentric breast cancer comprising of three different histopathological types are rare. Breast conserving surgery is a safe surgical option for multicentric breast cancer however the prognosis is usually poor due to advanced presentation and its tumor biology.
Acknowledgments
The authors would like to thank the Director General of Health Malaysia for his permission to publish this article.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/abs-19-101
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/abs-19-101). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhou MR, Tang ZH, Li J, et al. Clinical and pathologic features of multifocal and multicentric breast cancer in Chinese women: a retrospective cohort study. J Breast Cancer 2013;16:77-83. [Crossref] [PubMed]
- Qualheim RE, Gall EA. Breast carcinoma with multiple sites of origin. Cancer 1957;10:460-8. [Crossref] [PubMed]
- Middleton LP, Vlastos G, Mirza NQ, et al. Multicentric mammary carcinoma: evidence of monoclonal proliferation. Cancer 2002;94:1910-6. [Crossref] [PubMed]
- Taira N, Ohsumi S, Takabatake D, et al. Contrast-enhanced CT evaluation of clinically and mammographically occult multiple breast tumors in women with unilateral early breast cancer. Jpn J Clin Oncol 2008;38:419-25. [Crossref] [PubMed]
- Sardanelli F, Giuseppetti GM, Panizza P, et al. Sensitivity of MRI versus mammography for detecting foci of multifocal, multicentric breast cancer in Fatty and dense breasts using the whole-breast pathologic examination as a gold standard. AJR Am J Roentgenol 2004;183:1149-57. [Crossref] [PubMed]
- Bauman L, Barth RJ, Rosenkranz KM. Breast conservation in women with multifocal-multicentric breast cancer: is it feasible? Ann Surg Oncol 2010;17:325-9. [Crossref] [PubMed]
- Okumura S, Mitsumori M, Yamauchi C, et al. Feasibility of breast-conserving therapy for macroscopically multiple ipsilateral breast cancer. Int J Radiat Oncol Biol Phys 2004;59:146-51. [Crossref] [PubMed]
- Lim W, Park EH, Choi SL, et al. Breast conserving surgery for multifocal breast cancer. Ann Surg 2009;249:87-90. [Crossref] [PubMed]
- Gentilini O, Botteri E, Rotmensz N, et al. Conservative surgery in patients with multifocal/multicentric breast cancer. Breast Cancer Res Treat 2009;113:577-83. [Crossref] [PubMed]
- Egan RL. Multicentric breast carcinomas: clinical-radiographic-pathologic whole organ studies and 10-year survival. Cancer 1982;49:1123-30. [Crossref] [PubMed]
- Neri A, Marrelli D, Megha T, et al. Clinical significance of multifocal and multicentric breast cancers and choice of surgical treatment: a retrospective study on a series of 1158 cases. BMC Surg 2015;15:1. [Crossref] [PubMed]
Cite this article as: Mohamed Nazir MH, Ismail MS, Ismail IS, Ghazali MF, Thaumanavar CE, Ab Rahman KS, Wan Ab Rahman WI. Multicentric breast cancer comprising of three different histopathological types: a case report. Ann Breast Surg 2020;4:29.

