
Optimizing aesthetic results in free flap breast reconstruction: fat grafting and Hamdi’s Hammock
Introduction
Breast reconstructive surgery aims to recreate the female breast after its natural compounds and shape are lost in oncologic or preventive surgery. In autologous reconstruction, the remaining breast pocket is filled with an autologous tissue transfer (i.e., free flap surgery) or with fat grafting. Unfortunately, some properties of the breast gland are not simply replaced by those of adipose tissue. The surrounding breast pocket and footprint play an indispensable role in providing proper positioning and support for the adipose tissue inside. Consequently, common issues after reconstruction are related to a maldistribution of the new breast tissue. One of the most important landmarks in this regard is the position and definition of the inframammary fold (IMF). This intersection between the anterior breast capsule with the fascia superficialis of the pectoral muscles is often disrupted during oncologic breast surgery. It consists of a subcutaneous network of pseudo-ligamentous collagen bundles that connect the fascia to the skin, which creates an adherence visible as a fold (1). Methods for reconstruction of a disrupted or mal-positioned IMF goes back to 1977, when Pennisi anchored a dermal-fatty fascia flap to the deeper muscular fascia under open incision. Others anchored to the periosteum or the posterior capsule, but it wasn’t until 1990 that the IMF was reconstructed through the mastectomy pocket. The method of transcutaneously marking the IMF with needles dipped in methylene blue was introduced by Handel and Jensen to mark where they would put an interrupted unresorbable suture to anchor the subcutis and fascia superficialis to the thoracic wall. The running suture for this purpose was described by Nava, who also performed radial capsulectomy in the lower pole to obtain definition. A different way to determine the position of the suture was described by Chin and Pribaz, who used a Steinman pin to copy the shape of the contralateral IMF (2). The concept of thoracoabdominal tissue recruitment with internal suturing was effective and widely applicable in primary reconstruction or to resolve bottoming out (3). It is useful to create a fold, but it might fail to produce sufficient projection in the reconstructed breast. To obtain this, the tissues should be suspended upwards which creates a bulge that projects the breast forwards. This can be achieved by placing threads around the entire footprint of the breast in what is called the percutaneous purse string suture (PPSS) or Hamdi’s hammock (4). This paper provides a step-by-step guide with figures to master this surgical technique, including preoperative and postoperative management. The PPSS can be used with immediate lipofilling reconstruction or in combination with lipofilling to correct esthetically unpleasing results after autologous breast reconstruction. Its percutaneous nature avoids extra incisions and additional scars.
Surgical technique
Patient selection
The PPSS with lipofilling is indicated in patients that either were not eligible for free flap breast reconstruction or when secondary corrections are needed after free flap breast reconstruction. Patients must have a suitable donor site for fat grafting and be well informed about the varying degrees of fat graft retention, postoperative pain and possible suture failure or infection. Active smokers are asked to quit smoking at least 1 month before and after surgery.
Planning
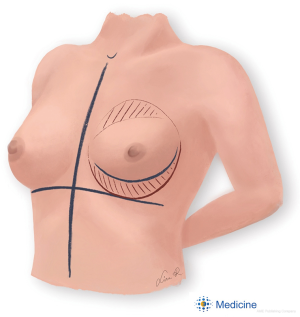
Preoperative markings are an essential step in breast surgery. They should be made with the patient standing up (Figure 1). The position of the IMF is defined as the most natural caudal tract of the breast footprint. The most caudal point of the curve lies midclavicular at the level of the 5th intercostal space. From this point the IMF curves medially towards the medial edge of the footprint, running 1–2 cm from the midline. The lateral curve runs in between the anterior axillary axis and midaxillary axis. The lipofilling donor sites are discussed with the patient and marked preoperatively, taking into account that the abdomen is closest to the surgical field and does not require additional tissue exposure or repositioning of the patient during surgery.
Surgical steps
The equipment needed for this procedure is a 10 mL Luer-Lock syringe, 2.0 polydioxanone suture (PDS), saline, a 19-gauge needle, a 15-blade scalpel and lipofilling canulae between 7 and 20 cm in length with a curved tip. The patient is installed in supine position with the arms tucked at the sides to avoid distortion of the breast. The lipofilling donor site is prepared with an infiltrative solution containing adrenaline and the lipoaspirate is collected in 10 cc Luer-Lock syringes for centrifugation at 1,200 rpm for one minute. After discarding the watery portion, the syringes are one by one connected to the lipofilling canula. During lipofilling, remaining retracting fibrous bands become more apparent and are resolved with extensive subcision to release the inferior pole of the breast pocket. A slight overcorrection of the wanted volume is advisory.
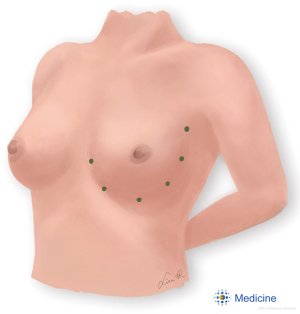
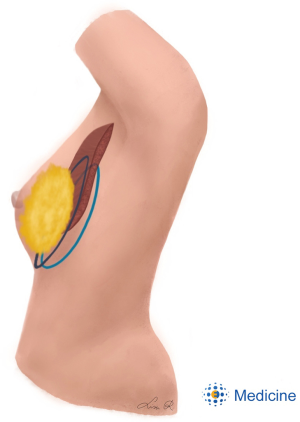
After completion of the lipofilling session, six small stab holes are created around the breast footprint (Figure 2). Two PDS sutures are guided around the breast footprint in two planes (Figures 3,4,5). The deep suture recruits tissue from the upper abdomen and suspends the IMF in an upward vector. This step allows the surgeon to determine the position of the IMF. The superficial suture encircles the breast footprint and defines the IMF more sharply by compressing the breast set-off in the inferior pole. This action tightens the fat graft pocket at its base, which bulges the tissue forward and improves breast projection.
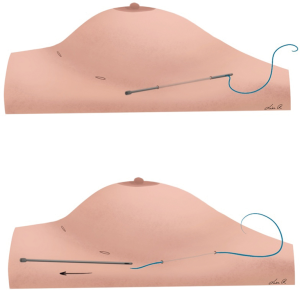

The knots are tightened with the patient in upright position to assess symmetry and shape. This allows finetuning of the IMF and adjusting the amount of breast projection. The suture trajectory runs more superficial around the stab holes, which can cause dimples. The tissue that is pulled down by the suture can be released by inserting a bent needle in the holes and lifting the skin. The resulted skin dimpling is smoothed down by freeing the superficial skin using a mosquito clamp through the stab incisions. Residual moderate dimpling will fade over time when the skin relaxes over 3–4 weeks after the surgery.
At the end of the procedure, a local anesthetic is infiltrated around the stab holes and in the 2nd–6th intercostal spaces on both sides of the breast.
Postoperative care
Patients are well informed that pain and feelings of tension are to be expected after this procedure and proper postoperative pain control should be foreseen. Antibiotic coverage is given for 5 days after the surgery. Patients are instructed to wear a supportive bra without underwire for 4 weeks starting 1 week after the procedure. They are advised to avoid pressure, cold contact, and abduction of the arms past 90 degrees for 2 weeks. In the follow up period, patients should be monitored for problems like pain, suture failure or suture infection. The procedure can be repeated if needed with an interval of at least 3 months.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Case series
Since 2011, a total of 312 patients have undergone PPSS to reconstruct the IMF, combined with either free flap-based surgery with lipofilling or lipofilling only in both partial and total breast reconstruction. The average age of the patients was 48 years (range, 29–68). A mean of 2 lipofilling sessions (range, 1–5) were performed and 65 (21% of total) patients needed a second PPSS procedure (never more than twice). No major postoperative complications occurred, however, three patients complained from significant persistent postoperative pain which never lasted more than 3 weeks. One suture broke at 4 weeks postoperatively as a result of overzealous physiotherapy. No suture exposure or infection occurred, but the knot was palpable in two thin patients.
Case 1
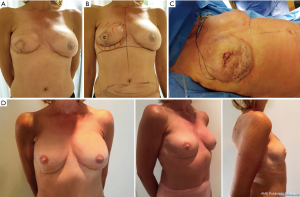
A 53-year-old woman received a reconstruction of the right breast by means of a free Mycutaneous Gracilis (TMG) flap. Afterwards, she showed a malpositioning of the IMF and lack of volume in the lower pole. Therefore, In the IMF was reconstructed using PPSS procedure with fat grafting to complete the reconstruction (Figure 6).
Case 2
A 55-year-old woman who underwent bilateral mastectomy received secondary autologous breast reconstruction by the means of bilateral TMG flaps. The patient refused to use her tummy as donor site for a free deep inferior epigastric artery perforator (DIEaP) flap. Secondary corrections were needed to enhance volume, projection and IMF positioning and definition using fat grafting and Hamdi’s Hammock. However, an additional session of fat grafting was planned after 3 months to improve the volume and contour of the reconstructed breasts (Figure 7).

Comments
PDS is a synthetic absorbable monofilament suture made from polyester. It reaches complete resorption after 200 days. During that time, it triggers a foreign body reaction that is visible as erythema and induration when running close to the skin. This explains why the sutures cause remnant of fibrosis along their trajectory. PDS will lose 80% of its tensile strength in 2 weeks and will be at 44% after 8 weeks. This allows the newly positioned tissues enough time to form adherence.
The use of percutaneous threads in fat grafting procedures of the breast was first presented by Khouri. In their method called reversed abdominoplasty and fat transfer (RAFT), upper abdominal tissue is recruited to the fat grafted breast by a superficial smooth suspension thread using sharp needles (5). Dr. Hamdi modified the technique to what named Hamdi’s Hammock using curved cannulae which resulted in safer technique (4).
Later on, Abboud et al. integrated the loops in his technique of no-scar breast reduction. He used PDS-0 loops to elevate the breast tissue and to fix the new IMF (6). More recently, Visconti and Salgarello described the use of barbed wires for breast footprint and IMF shaping in esthetic fat grafting in the breast. The dual anchored cog threads are introduced percutaneously using sharp needles and are guided back and forth along the inferior convexity of the breast footprint. This method uses compressive forces to better define or reposition the IMF. Also, they state that these threads might protect the borders of the breast footprint from loss of definition after postoperative edema (7).
The described technique in this paper combines a suspension suture in a superficial plane for IMF positioning and skin recruitment from the upper abdomen with a condensing suture under the pectoralis major for optimal IMF definition and improved breast projection.
To achieve optimal surgical outcomes, a few pearls and pitfalls should be kept in mind
Pearls:
- Proper preoperative planning: patient information, preoperative markings;
- When combined with fat grafting it is a minimal scar technique;
- The tension on the suture knots is determined with the patient in sitting position;
- Subcision is an indispensable step to release the fibrous bands that define the old, malpositioned IMF and to release the breast pocket where needed;
- In bilateral reconstruction, the knots are tied simultaneously at both sides to obtain symmetrical results;
- The sutures encircling the breast should be passed on or just outside the intended breast footprint. Insertion of the suture in the inside of the footprint should be avoided, since this will be exacerbated after tightening the knots;
- The knots are tied and buried on the anterior axillary axis;
Pitfalls:
- Inadequate postoperative pain management;
- Avoid causing trauma to the thoracic wall by staying perpendicular to the muscular plan. Blind passages in the wrong plane might cause pneumothorax;
- Overtightening the sutures will cause unnecessary postoperative pain and pressure the soft tissues;
- Monofilament sutures should be knotted properly to avoid early suture failure.
Acknowledgments
Artworks are courtesy of L Ramaut, MD.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Edward I. Chang) for the series “Novel Innovations and Advancements in Breast Reconstruction” published in Annals of Breast Surgery. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/abs-20-69). The series “Novel Innovations and Advancements in Breast Reconstruction” was commissioned by the editorial office without any funding or sponsorship. Both authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bogetti P, Cravero L, Spagnoli G, et al. Aesthetic role of the surgically rebuilt inframammary fold for implant-based breast reconstruction after mastectomy. J Plast Reconstr Aesthet Surg 2007;60:1225-32. [Crossref] [PubMed]
- Kraft CT, Rendon JL, Koutz CA, et al. Inframammary Fold Reconstruction in the Previously Reconstructed Breast: A Comprehensive Review. Plast Reconstr Surg 2019;143:1019-29. [Crossref] [PubMed]
- Khouri RK, Rigotti G, Khouri RK Jr, et al. Tissue-engineered breast reconstruction with brava-assisted fat grafting: A 7-year, 488-patient, multicenter experience. Plast Reconstr Surg 2015;135:643-58. [Crossref] [PubMed]
- Hamdi M, Anzarut A, Hendrickx B, et al. Percutaneous purse-string suture: An innovative percutaneous technique for inframammary fold creation and improved breast projection in reconstructive surgery. Aesthet Surg J 2018;38:1298-303. [Crossref] [PubMed]
- Khouri RK, Cardoso E, Rotemberg SC. The reverse abdominoplasty and fat transfer (RAFT) procedure: A minimally invasive, autologous breast reconstruction alternative. Isle of Ischia, Italy: Presented at the 25th Meeting of the European Assiciation of Plastic Surgeons (EURAPS), 2014.
- Abboud MH. No scar reduction mammaplasty: 3 years experience. Madrid Spain: Presented at the 29th Meeting of the European Association of Plastic Surgeons (EURAPS), 2018.
- Visconti G, Salgarello M. Dual-Anchor Cog Threads in Fat Grafting Breast Augmentation: A Novel Scarless Method for Defining Breast Footprint and Enhancing Shape. Plast Reconstr Surg 2019;143:1039-49. [Crossref] [PubMed]
Cite this article as: Ramaut L, Hamdi M. Optimizing aesthetic results in free flap breast reconstruction: fat grafting and Hamdi’s Hammock. Ann Breast Surg 2020;4:28.

