Exceedingly rare lactating adenoma of 3-year duration: a case report
Introduction
Lactating adenoma (LA) is a benign tumor of pregnancy that usually presents in the primigravida woman in her 2nd or 3rd decade (1). Palpable benign masses during pregnancy and lactation are common due to breast enlargement and hormonal changes. As such, lactating adenomas most often regress spontaneously after cessation of breast feeding (2). They usually presents as a firm, mobile and painless mass in the upper outer quadrant of the breast and falls within a differential diagnosis consisting of fibroadenoma, galactocele or lobular hyperplasia but malignancy, although rare, needs to be ruled out (1-3). LA are benign stromal variations caused by physiological changes during pregnancy and lactation (2,4). Lactating adenomas have been described as tubular adenomas with secretory changes that occur during pregnancy and lactation (5). The diagnosis is traditionally with ultrasound due to the ability to differentiate between solid and cystic masses, its lack of radiation exposure and its usefulness for guidance for core needle biopsies (2,6). However, LA can be difficult to distinguish from other benign breast tumors sonographically. It appears as a well-defined, smooth, oval mass that is hypoechoic with posterior acoustic enhancement or as a hyperechoic mass with internal vascularity (1,5,6). LA are generally observed and tend to only be excised if there is concern for a coinciding malignancy or for cosmesis (2,7). We present a rare case of a persisting lactating adenoma for the duration of 3 years despite cessation of lactation. We present the following article in accordance with the CARE reporting checklist (available at https://abs.amegroups.com/article/view/10.21037/abs-20-144/rc).
Case presentation
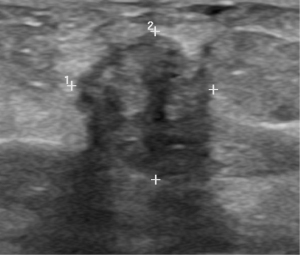
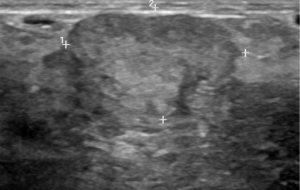
A 29-year-old female, Gravida 1 Para 1, presented 1 month postpartum and while still breastfeeding with a left breast lump that had been present for 8 months. She was otherwise asymptomatic with no pain, skin or nipple changes. She denied any personal history of breast cancer or breast disease. Careful examination revealed a 2 cm firm and rounded nodule in the superior central aspect of her left breast. No enlarged axillary nodes were detected. An ultrasound exam reported a circumscribed hyperechoic mass with internal blood flow measuring 2.5 cm × 2.4 cm × 1.7 cm. An ultrasound-guided large core needle biopsy was performed. Pathology specimen proved to be a lactating adenoma with no evidence of atypic or malignancy. After lactation ceased the mass partially regressed but remained palpable (Figure 1). One of the diagnostic challenges of this case was patient compliance with follow-up. The patient was lost to follow up for 2 years and then presented to the clinic after delivering her second child. She presented with the same left breast mass now larger in size and stated that the mass never fully resolved and remained palpable for the past 2 years. Another diagnostic challenge of this case was the ability to exclude malignancy. Ultrasound after the 2 years revealed a well-defined left breast mass containing previous biopsy clip at 12:00 axis measuring 2.7 cm × 2.3 cm × 1.6 cm (Figure 2). Patient continued to undergo biannual ultrasound examinations that revealed a persistent hypoechoic mass with clear margins and no posterior shadowing despite cessation of breastfeeding. Therefore, surgical excision was warranted. Patient underwent open biopsy with ultrasound guidance of the mass. Pathology revealed the presence of a tubular adenoma without evidence of malignancy in our nonlactating patient (Figure 3). Patient did well post-operatively without any adverse or unanticipated events. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Discussion
LA is one of the common benign tumors of pregnancy and lactation along with galactocele, fibroadenoma, and lobular hyperplasia (1,5). Lactation adenomas do not have any malignant potential, however, any solid breast mass in pregnant patients should be biopsied as up to 3% of breast cancer is diagnosed in pregnancy and lactation (5,8,9). Lactating adenomas are thought to form due to the hormone associated proliferation and formation of tubulo-alveolar structures of the breast. During pregnancy, there are high concentrations of progesterone, estrogen and prolactin that promote this high proliferative activity (2). LA is characterized by secretory epithelium that resemble the physiologic changes during lactation. They are formed by lobulated masses of expanded acini that are separated by thin vascular septations and surrounded by edematous stroma (10). These lobules are filled with colostrum and fat and lined by cuboidal epithelial cells (1). In the literature, lactating adenomas and tubular adenomas have been reported as the same entity. LA have been described as tubular adenomas with secretory changes that occur during pregnancy and lactation (5,11). This is highlighted in our presented case. The core needle biopsy performed during lactation revealed a LA and the excision performed after cessation of breastfeeding was interpreted as a tubular adenoma, essentially a LA without secretory changes.
Generally, LA are firm, painless, well-circumscribed lesions that usually present in the upper outer quadrant and range from 2–4 cm (1,7,10). Mammography is not recommended during pregnancy due to radiation exposure and its sensitivity and specificity are limited by high breast density during this time (5). Ultrasonography is the main diagnostic tool of a breast mass using during pregnancy due to its accuracy and safety profile (1). However, the diagnostic features of LA on ultrasound are common to a variety of benign lesions. LA are generally described as having an ovoid shape with smooth borders, posterior acoustic enhancement, and being a well-circumscribed hypoechoic solid mass (6). Therefore, lactating adenomas are difficult to distinguish from other benign breast lesions. LA can only be definitively diagnosed with a thorough history, physical examination, and a histopathological specimen. Most lactating adenomas spontaneously involute. In 5% of cases, LA infarct due to the relative vascular insufficiency in the lactating breast (10). As lactating adenomas tend to spontaneously regress, they require no additional treatment. However, if producing severe pain, become disfiguring or if there is concern for concomitant malignancy, surgical excision is warranted. Bromocriptine, a Dopamine agonist, has been used to decrease the size of lactating adenomas prior to surgical excision (12). This case demonstrates a woman whose LA did not involute or infarct but rather persist for 3 years. The limitation of this case was poor patient compliance with follow up. Had the patient been able to regularly follow up in the office, the previously biopsied mass could have been sonographically followed to objectively document its presence for the 2-year duration. In review of the literature, we present the longest persisting lactating adenoma. This case highlights that surgical excision is the only method to exclude co-existing malignancy reliably and accurately in cases of lactating adenomas that do not regress.
Conclusions
Lactating adenomas are benign stromal variations that occur during the physiologic changes of pregnancy. Similar to all solid tumors of pregnancy and lactation, LA require a comprehensive evaluation to rule out malignancy. A thorough work up includes a history, physical, imaging, and histological findings. LA most often regress spontaneously after the cessation of breastfeeding. We present a rare case report of the longest persisting lactating adenoma reported in the literature. This case highlights that surgical excision is warranted when there is failure of regression to exclude malignancy accurately and reliably.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://abs.amegroups.com/article/view/10.21037/abs-20-144/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://abs.amegroups.com/article/view/10.21037/abs-20-144/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kumar K, Reddy C, Swarupa R, et al. Lactating adenoma of the breast: A case report. IAIM 2015;4:161-5.
- Magno S, Terribile D, Franceschini G, et al. Early onset lactating adenoma and the role of breast MRI: a case report. J Med Case Rep 2009;3:43. [Crossref] [PubMed]
- Hamza A, Idris S. Lactating Adenoma of the Breast a Diagnostic Difficulty in Pregnancy and Rewarding Natural History during Lactation: A Case Report and Review of Literature. Med J 2014;1:13-6.
- de Holanda AA, Concalves A, de Medeiros R, et al. Ultrasound findings of the physiological changes and most common breast diseases during pregnancy and lactation. Radiol Bras 2016;49:389-96. [Crossref] [PubMed]
- Yu JH, Kim M, Cho H, et al. Breast diseases during pregnancy and lactation. Obstet Gynecol Sci 2013;56:143-59. [Crossref] [PubMed]
- Barco Nebreda I, Vidal M, Fraile M, et al. Lactating Adenoma of the Breast. Journal of Human Lactation 2016;32:559-62. [Crossref] [PubMed]
- El Fazazi H, Benabdejlil Y, Achenani M, et al. Lactating Adenoma: A case report. International Journal of Innovation and Applied Studies 2014;7:1671-1673.
- Han BY, Li X, Zhao H, et al. Clinical features and survival of pregnancy-associated breast cancer: a retrospective study of 203 cases in China. BMC Cancer 2020;20:244. [Crossref] [PubMed]
- Collins JC, Liao S, Wile A. Surgical management of breast masses in pregnant women. J Reprod Med 1995;40:785-8. [PubMed]
- Baker TP, Lenert J, Parker J, et al. Lactating adenoma: a diagnosis of exclusion. Breast J 2001;7:354-7. [Crossref] [PubMed]
- Volckmar AL, Leichsenring J, Flechtenmacher C, et al. Tubular, lactating, and ductal adenomas are devoid of MED12 Exon2 mutations, and ductal adenomas show recurrent mutations in GNAS and the PI3K–AKT pathway. Genes Chromosomes Cancer 2017;56:11-7. [Crossref] [PubMed]
- Szabo J, Garcia D, Ciomek N, et al. Spuriously aggressive features of a lactating adenoma prompting repeated biopsies. Radiol Case Rep 2017;12:215-8. [Crossref] [PubMed]
Cite this article as: Layton C, Melnikau S, Collado-Mesa F, Avisar E. Exceedingly rare lactating adenoma of 3-year duration: a case report. Ann Breast Surg 2022;6:10.