An update on breast animation deformity grading systems—a systematic review
Introduction
Breast animation deformity (BAD) is a common and afflicting sequelae of breast reconstruction or augmentation, and is estimated to occur with variable severity in anywhere from zero to 75% of reconstructions/augmentation (1). It is characterized by an unsightly deformation, a motion deformity, resulting in displacement of the implant and skin rippling associated with contraction of the pectoral muscle (2). BAD is an aesthetic concern, as well as a functional problem. Muscle twitching, pain, and impaired shoulder function are significant problems, especially in physically active women—thus affecting patient’s health-related quality of life (HR-QOL) (3-5).
BAD is seen following submuscular implant placement in both breast augmentation and reconstruction. Concurrently, patients with submuscular breast augmentation or reconstruction have reported more pain compared to patients with premuscular/prepectoral augmentation or reconstruction (6,7). In a previous review from our department we postulated, that the degree of BAD seemed proportional to the degree of muscle involvement in implant-based breast reconstruction or augmentation (8). This means that the degree of BAD seems to be proportional to the surface area of implant covered by muscle. Total coverage seems to be associated with the most severe degree of BAD and gradually diminishes over dual-plane to triple plan techniques and seems negligible with no muscle coverage. However, evidence is still limited regarding the etiology of BAD (9,10). Furthermore, we assessed four different grading systems available at that time, and the surgical techniques used in the included studies (8). None of the existing grading scales were appraised useful for clinical purposes (1,11-13). The topic ‘animation deformity’ has subsequently gained more attention, and numerous studies have been conducted to assess the etiology, treatment and grading systems of BAD (9,14-18).
This study is the newest update and a further development of our previous systematic review. The aim of this review was to critically appraise the various grading systems available to evaluate BAD, and to investigate the quality and reproducibility of the individual grading systems in the search of the optimal grading scale. In addition, we estimate the prevalence of BAD following either breast augmentation or reconstruction. Finally, we wish to discuss the applicability of BAD assessment tools in daily clinical practice and for scientific purposes. We present the following article in accordance with the PRISMA reporting checklist (available at https://abs.amegroups.com/article/view/10.21037/abs-21-46/rc) (19).
Methods
This review has been registered in the International Prospective Register of Systematic Reviews (PROSPERO) with the registration number: CRD42021223940.
Literature search strategy
In October 2020 a systematic literature search was conducted according to PRISMA Guidelines (19) in the following electronic databases: PubMed (National Library of Medicine, NLM), Embase Classic (Ovid), and Embase (Ovid). The following terms was used in the search strategy: ((direct-to-implant) OR (breast implant) OR (breast implantation) OR (breast reconstruction) OR (breast augmentation) OR mammaplasty OR mastoplasty OR (breast enlargement) OR (breast prosthesis) OR (breast enhancement)) AND ((implant placement) OR (pre pectoral) OR subpectoral OR (pre pectoral hammock) OR subglandular OR submuscular OR premuscular OR subfascial OR (direct-to implant) OR (pectoralis muscles) OR (dual-plane) OR (triple-plane)) AND (distortion OR deformation OR (animation deformity) OR (breast deformation) OR contraction OR elevation OR displacement OR malposition OR cosmetic OR aesthetic OR appearance OR rippling). Only studies in English, Danish or German were included, with no time limitations.
The reference list of included papers was subsequently hand searched for additional studies.
The literature search was conducted in Covidence (https://www.covidence.org). First, a title and abstract screening was conducted. Studies evaluating “breast animation deformity”, “implant-based breast augmentation”, or “immediate breast reconstruction” were considered candidate studies for further evaluation based on the inclusion and exclusion criteria established prior to the literature search.
Eligibility criteria
Studies were selected if published as full-text papers and if the objective of the studies were assessment or quantification of BAD. Studies, that did not define how BAD was assessed were not considered eligible.
Inclusion criteria:
- Study design: prospective, retrospective, randomized controlled trials, systematic reviews;
- Assessment of BAD objective and subjective assessment;
- Language requirements: English, Danish, or German.
Exclusion criteria:
- Study design: Case-reports;
- Other languages then the above named;
- Not defining or assessing BAD;
- Studies that focused on most appropriate implant type, and not complications or BAD;
- Studies that only included reoperations;
- Studies that focused on treatment of BAD, thus did not define BAD.
Study selection and data extraction
Full-text of candidate studies were retrieved and screened by two independent authors (J.B.T. and F.D.). Conflicts were resolved by consensus of the two reviewers and, if necessary, a third author (J.A.S). For all eligible studies, the same two reviewers (F.D and J.B.T.) extracted data. All included studies were reviewed using a descriptive checklist including authors, publication country, year, study design, sample size, patient demographics, see Table 1. The quality of the included studies was assessed with a checklist developed by our study group in regards of: (I) Description of study sample, (II) rate of participation, (III) surgical technique description, (IV) follow-up period, (V) assessment of BAD, (VI) grading, classification or quantification of BAD, and (VII) reproducibility of the assessment of BAD. The quality of each study is represented with a total score between zero to seven (zero with the lowest quality, and seven with highest quality).
Table 1
| Author, year | Country/region | Type of study | No. of participants | Method of data collection | Data assessors | Duration of follow-up (mo) | Outcome variable |
|---|---|---|---|---|---|---|---|
| Pelle-Ceravolo, 2004, (12) | Italy | Retrospective | 348/580 | Psychical exam, 6 judgements for each patient | Surgeon, nurse, patient | 6 | BAD |
| Spear, 2009, (1) | United States | Case-series | 40/40, 69/195 | Photographs, questionnaire (non-validated) | Plastic surgery residents, patient | 6 | BAD, self-evaluation of BAD |
| Bracaglia, 2013, (11) | Italy | Retrospective | 524 | Photographs, physical exams | Plastic surgeon | 6–180 | BAD |
| Nigro, 2017, (13) | USA | Retrospective | 84/108 | Questionnaire | Patient | 6–72 | BAD, level of physical activity |
| Dyrberg, 2019, (14) | Denmark | Retrospective | 37 (74 breasts) | Video | Plastic surgeons | 16 (476 days) | BAD, inter- and intraobserver agreement |
| Vidya, 2018, (18) | United Kingdom | Descriptive, review | N.S. | Photographs, Video | N.S | N.S. | Classification of BAD |
| Kim, 2019, (15) | Taiwan | Prospective, cross-sectional | 88 (145 breasts) | Video | ImageJ analysis Physician |
17.7 | Quantification of BAD |
| Becker, 2017, (4) | United States | Cross-sectional study | 25 | Chart reviews, questionnaire, physical examination | Physical examination by senior author and medical student | N.S. | Classification of BAD, quality of life |
| Bracaglia, 2020, (9) | Italy | Retrospective | 605 | Photographs, physical examination | Plastic surgeons | 6, 12, 80 | Classification of BAD, Breast-Q |
| Kümmel, 2018, (17) | Germany | Descriptive | N.S. | Physical examination, photographs, N.S. | N.S. | N.S. | Classification of BAD |
| Dyrberg, 2019, (8) | Denmark | Systematic review | 4 studies | Systematic review | Pelle-Ceravolo, Spear, Bracaglia, Nigro grading system | 6–180 | BAD |
| Fracol, 2019, (20) | United States | Overview | 3 studies | Overview | ImageJ analysis, physician |
N.S. | Classification of BAD, treatment of BAD |
| Fracol, 2020, (16) | Taiwan | Prospective | 141 | Video | ImageJ analysis, physician | 3–113 | BAD, BREAST-Q |
BAD, breast animation deformity; N.S, not specified; mo, months.
Results
Eligible studies
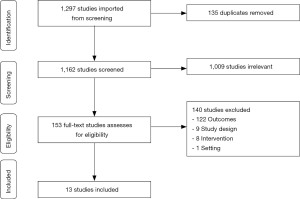
The literature search yielded 1,297 studies imported for screening, reduced to 1,162 after duplicates were removed. These studies were reviewed as described in methods by two independent reviewers, 13 studies met the inclusion criteria and were included in this systematic review (1,4,8,9,11-18,20). The process of selecting eligible studies is listed in Figure 1, PRISMA flowchart.
Study characteristic
Descriptive characteristics of included studies are summarized in Table 1. Studies were published from 2004 to 2020. The study designs were retrospective, prospective, cross-sectional, descriptive studies, systematic reviews or overviews. The number of participants in the included studies ranged from 25 to 605. The age of participants was described in seven studies (4,9,11,13-16), with a median age ranging from 33.6 to 49.7 years. There were various variations of BAD assessments from surgeon evaluations, patient self-evaluation to quantification with imaging software (ImageJ) for analysis of BAD. Four of the six studies using patient-reported outcomes used non-validated questionnaires (1,4,13,15), whereas two studies used the validated BREAST-Q (9,16). The follow-up period ranged from three months to 15 years. Out of the 13 included studies, four studies were evaluated in previous review (1,11-13), five new grading systems were suggested (4,14,15,17,18), three studies reused or modified the existing grading systems (9,16,20), and one systematic review (our previous review) did not suggest a new grading systems, but evaluated the quality of the four previously described grading scales (8).
Study quality
Twelve studies had a clear description of the study (1,4,8,9,11-16,18,20), one study presented a grading system without a clear definition of the study (17). The participation rate was described in 11 studies. Two studies consisted of a systematic review and an overview with a description of number of studies or participant rates in the included studies (8,20), while three studies did not define participant rates or number of studies (11,17,18). Three studies did not describe the surgical technique used (4,17,20). Only four studies defined their follow-up period in the group (9,14,15,21), whereas the remaining studies had different follow-up on patients (1,4,8,11-13,16-18,20). BAD was assessed by competent assessors in 10 studies (1,4,8,11,12,14-16,20,21), three studies did not define who assessed BAD (9,17,18), and one study only used patient-self assessment of BAD (13), using a non-validated questionnaire. Six studies assessed patient-reported outcomes (1,4,9,15,16) of which only two studies used validated questionnaires (9,16). Thirteen studies had a well-defined grading system of BAD (1,4,8,9,11-18,20), however three studies reused existing grading systems (9,16,20). Only three studies examined whether their findings were reproducible (14,15,21). The quality of studies is presented in Table 2.
Table 2
| Author, year | Clear description of study | Participation rate | Description of surgical technique | Similar follow-up | Competent assessment of BAD | Definition of BAD | BAD definition reproducible? | Total score |
|---|---|---|---|---|---|---|---|---|
| Pelle-Ceravolo, 2004, (12) | Yes | Yes | Yes | No | Yes | Yes | No | 5/7 |
| Spear, 2009, (1) | Yes | Yes | Yes | No | Yes | Yes | No | 5/7 |
| Bracaglia, 2013, (11) | Yes | No | Yes | No | Yes | Yes | No | 4/7 |
| Nigro, 2017, (13) | Yes | Yes | Yes | No | Patient self-assessment | Yes | No | 5/7 |
| Dyrberg, 2019, (14) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 7/7 |
| Vidya, 2018, (18) | Yes | No | Yes | No | No | Yes | No | 4/7 |
| Kim, 2019, (15) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 7/7 |
| Becker, 2017, (4) | Yes | Yes | No | No | Yes | Yes | No | 4/7 |
| Bracaglia, 2020, (9) | Yes | Yes | Yes | Yes | No | Yes | No | 5/7 |
| Kümmel, 2018, (17) | No | No | No | No | No | Yes | No | 1/7 |
| Dyrberg, 2019, (8) | Yes | Yes | Yes | No | Yes | Yes | No | 5/7 |
| Fracol, 2019, (20) | Yes | Yes | No | No | Yes | Yes | No | 3/7 |
| Fracol, 2020, (16) | Yes | Yes | Yes | No | Yes | Yes | No | 5/7 |
BAD, breast animation deformity.
Surgical technique
The surgical techniques used varied across studies. The surgical technique of Pelle-Ceravolo et al. (12), Spear et al. (1), Nigro et al. (13), and Bracaglia et al. (11) were all subpectoral implant placement and is described in our previous review (8). In brief, Pelle-Ceravolo described breast augmentation using either the Regnault technique or a dual-plane muscle-split technique (12). Spear et al. used a dual-plane partial muscle coverage technique (1), and Bracaglia a triple-plane technique (11). Nigro used a dual-plane technique for patients undergoing either direct-to-implant or two-stage immediate breast reconstruction with the use of acellular dermal matrix (ADM) in the lower pole (13). Since then, six new studies described their surgical techniques while assessing or grading BAD (9,14-16,18,22). Bracaglia et al. (2019) presents a triple-plane technique, as described in their previous study, and added either a bra flap or an inverted bra flap modified dual plane technique. (9). Vidya et al. (2018) and Kim et al. both briefly described a subpectoral implant placement using either a bra flap or a hammock-based technique using an ADM (15,18). Fracol et al. used a subpectoral implant placement, where the pectoralis major muscle was divided along its inframammary and medial border (16). Dyrberg et al. used either a subpectoral (dual-plane) implant placement or prepectoral placement of implant (14), both techniques are recently published in visualized articles (23,24). No other studies evaluated prepectoral implant placement and BAD (1,4,8,9,11-13,15-18,20).
Update on BAD grading systems
In our previous review we described the four existing grading scales available; consisting of Pelle-Ceravolo et al. (12), Spear et al. (1), Bracaglia et al. (11) and Nigro et al. (13). None of the available grading systems examined their grading scales for reproducibility. Only Spear’s grading system was deemed useful for clinical purpose, as it was the only grading system tested for assessment of BAD in a clinical setting (1). Since then, five new grading systems were suggested; Dyrberg et al. (14), Vidya et al. (18), Kim et al. (15), Becker et al. (4) and Kümmel et al. (17). Three out of the five new grading systems used a 3-point scale (14,15,17), while two studies used a 4-point scale (4,18). The different grading systems are presented in Table 3.
Table 3
| Author, year | Class I | Class II | Class III | Class IV | Other |
|---|---|---|---|---|---|
| Pelle-Ceravolo, 2004, (12) | Non-existing or minimal deformity | Moderate deformity with a certain alteration of the breast shape but with limited effect on the aesthetic appearance of the breast | Important and obvious deformity that was definitely aesthetically unacceptable | ||
| Spear, 2009, (1) | No distortion and unable to discern whether the implant lie in front of or behind the pectoralis muscle | One is able to tell that the implant is subpectoral, but there is minimal distortion with an aesthetically pleasing result | Moderate distortion but still an aesthetically acceptable result | Severe distortion with an unattractive result during muscle contraction | |
| Bracaglia, 2013, (11) | No distortion and unable to discern whether the implant lie in front of or behind the pectoralis muscle | One is able to tell that the implant is subpectoral, but there is minimal distortion with an aesthetically pleasing result | Moderate distortion but still an aesthetically acceptable result | Severe distortion with an unattractive result during muscle contraction | |
| Nigro, 2017, (13) | Twicthing or movement of the upper pole of the breast with certain muscle movement of the arms or chest | If yes, how bothersome do you find it on a scale of 1 to 10 where 1 is not at all and 10 being disabling | Converted to categories: minimal: 1–2.5; mild: 3–5; moderate: 5.5–7.5; severe: 8–10 | ||
| Dyrberg, 2019, (14) | TBM/NAC distortion: no distortion (0 points) | TBM/NAC distortion: visible distortion (1 point). TBM/NAC moves upwards, but remains in a vertical position | TBM/NAC distortion: severe distortion (2 points). TBM/NAC moved upwards, horizontalized and kinked inwards | NSE grading system | |
| Breast skin distortion: no distortion (0 points) | Breast skin distortion: visible distortion (1 point); breast skin is slightly wrinkled, with wrinkles apparent in only on quadrant | Breast skin distortion: severe distortion (2 points). Breast skin was wrinkled with long horizontal lines affecting more than one quadrant | ● Distortion of the TBM/NAC (0–2 points); | ||
| ● Distortion of the breast skin surrounding the TBM/NAC (0–2 points); | |||||
| ● Distortion of the entire breast (0–2 points) | |||||
| Breast movement: no movement (0 points) | Breast movement: visible movement (1 point). Movement of the entire breast, the whole breast lifted upwards, revealing a visible inframammary crease | Breast movement: severe movement (2 point). Movement of the entire breast resulting in the whole breast lifted upwards and revealing more than a visible inframammary crease | Total 0–6 points | ||
| Vidya, 2018, (18) | No visible distortion and displacement of the implant during muscle contraction, both during normal and exercise activity | Minimal visible distortion with displacement of the implant (superolaterally) during muscle contraction both in normal and exercise activity, grooving may be seen, unnoticed by patient | Moderate visible distortion during muscle contraction, with displacement of the implant (superolaterally) during muscle contraction both during normal and exercise activity, often noticed by patient | Severe distortion during muscle contraction with persistent displacement of the implant both in normal and exercise activity, unattractive results disturbing the patient | |
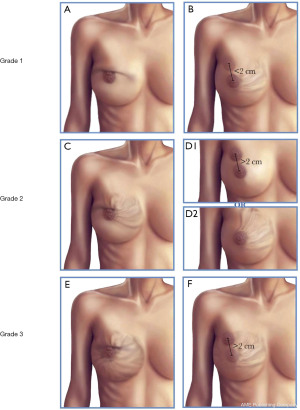
| Kim, 2019, (15) | Patients have less than 2 cm nipple displacement and less than 25% (one-quarter of the breast mound) are of skin contour irregularity (rippling) | Patients have either greater than 2 cm nipple displacement or more than 25% surface area of skin rippling | Patients have both greater than 2 cm nipple displacement and 25% surface area skin rippling | ||
| Becker, 2017, (4) | Minimal breast distortion, minimal lateral displacement, and minimal to no skin rippling | Moderate breast distortion, moderate lateral displacement or elevation, and minimal rippling | Moderate to severe breast distortion, moderate to severe lateral displacement or elevation, and evident skin rippling | Severe deformity, symmetric breasts with severe lateral or superior displacement, and severe skin rippling | |
| Bracaglia, 2020, (9) | No distortion and no ability to discern whether the implant lay behind or in front of the pectoralis muscle | Ability to tell that the implant was subpectoral, with mild distortion but an aesthetically pleasing result | Moderate distortion, but still an aesthetically acceptable result | Severe distortion with an unattractive result during muscle contraction |
NSE, Nipple, Surrounding Skin, Entire Breast; TBM, top of the breast mound; NAC, nipple areolar complex.
Prevalence of BAD and surgical types
Eight studies assessed the prevalence of BAD in their study population using their suggested grading system (self-assessments were not included in this analysis) (1,4,9,11,12,14-16). The total number of patients assessed for BAD was 1,894 in this systematic review. The total prevalence of patients with some degree of BAD (mild, moderate or severe) was 73.3%. We excluded grading scales where grade 1 consisted of none to minimal BAD in the calculation of the total prevalence of BAD. The degree of BAD varied from 10% (22) to 94.7% (14). See Table 4 for prevalence of BAD in each study.
Table 4
| Author | Subpectoral and used grading system | Outcome | Prepectoral and used grading system | Outcome |
|---|---|---|---|---|
| Pelle-Ceravolo, 2004, (12) | Muscle-split prepectoral (n=1,812a) | I: 69.5 (1,261/1,812); II: 24.9 (452/1,812); III:5.4 (99/1,812); total: 30.4 (551/1,812) | ||
| Regnault technique (n=276b) | I: 26.8 (74/276); II: 25.7 (71/276); III: 47.4 (131/276); total: 73.1 (202/276) | |||
| Spear, 2009, (1) | Spear’s grading system (n=40) | I: 22.5 (9/40); II: 62.5 (25/40); III: 10 (4/40); IV: 5 (2/40); total II−IV: 77.5 (31/40) | ||
| Self-evaluation (n=69) | None-mild: 82(56/69); moderate: 10 (7/69); severe: 7 (5/69); total: 24.6 (17/69 | |||
| Bracaglia, 2013, (11) | Bracaglia’s grading system (n=524) | I: 67 (351/524); II: 29.7 (156/524); III: 3 (17/524); IV: 0 (0/524); total: 33.0 (173/524) | ||
| Nigro, 2017, (13) | Self-questionnaire (n=84) | None: 24.4 (20/84); mild: 50 (41/84); moderate: 14.6 (12/84); severe: 11 (9/84); total: 73.8 (62/84) | ||
| Dyrberg, 2019, (14) | NSE grading system (n=19) | Surgeon 1: 1th: 4±1, 2th: 5.1±1.1 Surgeon 2: 1th: 3.8±1.1, 2th: 4.2±1.2 NSE: 4.3±1.1 Total NSE >2: 94.7 (18/19) |
NSE grading system (n=18) | Surgeon 1: 1th: 0.2±0.6, 2th: 0.3±0.6 Surgeon 2: 1th: 0.2±0.7, 2th: 0.1±0.4 NSE: 0.2±0.6Total NSE >2: 10.5 (2/19) |
| Kim, 2019, (15) | Kim’s grading system (n=145b) | I: 41.4 (60/145); II: 35.9 (52/145); III: 22.8 (33/145); total: 58.6 (85/145) | ||
| Subjective grading (Becker’s subjective grading) (n=145b) | Grade 1: 40.0 (58/145); grade 2: 35.2 (51/145); grade 3: 18.6 (27/145); grade 4: 6.2 (9/145); total: 60.0 (87/145) | |||
| Becker, 2017, (4) | Becker’s grading system (n=25) | I: 20 (5/25); II: 40 (10/25); III: 24 (6/25); IV: 12 (3/25); total: 76.0 (19/25) | ||
| Subjective grading (n=20) | Grade 1−2: 25 % (5/20); grade 3−5: 30 (6/20); grade 6+: 45 (9/20); total: 75.0 (15/20) | |||
| Bracaglia, 2020, (9) | Spear’s grading system (n=605) | I: 73.8 (444/605); II: 31.1 (188/605); III: 3.3 (21/605); IV: 0 (0/605); total: 34.5 (209/605) | ||
| Fracol, 2020, (16) | Kim’s grading system (n=86) | I: 34.9 (30/86); II: 36 (31/86); III: 29.1 (25/86); total: 65.1 (56/86) |
Values are presented in percentage (number cases/number in total). a, 302 patients × 6 judgements =1,812; b, 46 patients × 6 judgements =246. NSE, Nipple, Surrounding Skin, Entire Breast.
The prevalence of BAD in the prepectoral group was 10.5% (14). Eight studies assessed BAD in subpectoral implant placement, where the prevalence of BAD were 73.9% (1,4,9,11,12,14-16). The highest prevalence of BAD was found in subpectoral implant placement; dual-plane muscle splitting technique used in Spear et al. (prevalence of 78%) (1), Regnault technique used in Pelle-Ceravolo et al. (prevalence of 73%) (12) and Becker et al. (prevalence of 76%) where the surgical technique was not further elaborated (4). The Regnault technique had a prevalence of 47% of severe BAD, as in our previous review (12). Dyrberg et al. assessed BAD with Nipple, Surrounding Skin, Entire Breast (NSE) grading scale (0–6 points), where the prepectoral group had NSE score on 0.2±0.6, while the subpectoral group had NSE score on 4.3±1.1 (14). With supplementary data from the research group, 18 out of 19 patients with subpectoral implant placement had some degree of BAD, a total NSE score of >2, while only two patients in prepectoral implant placement had a NSE score of >2, resulting in a prevalence of BAD of respectively 94.7% (subpectoral) versus 10.5% (prepectoral) in each group.
Discussion
This systematic review is the newest update on BAD grading systems, an evaluation and quality assessment of the existing grading scales, and the prevalence of BAD in regards of implant placement and type of surgical technique. We retrieved 1,297 studies of which 13 studies were included in this review. Since our previous review, five new grading systems have been presented. Only two grading systems scored a maximum of 7 out of 7 points in the quality assessment of studies and grading system; our own NSE grading scale and Kim et al.’s grading system. We found significantly higher prevalence of BAD in the subpectoral implant placement group than the prepectoral implant placement group (73.9% versus 10.5%). There was no evidence of a specific type of surgical technique in the subpectoral group would result in higher prevalence of BAD. The total prevalence of moderate to severe BAD was 73.3% in this systematic review.
The grading systems of Kim et al. (15) and Dyrberg et al. (14) were both rated high in quality in the quality checklist, with a total score of 7 out of 7 total points with a clear description of the grading systems, competent assessment of BAD, clear definition of BAD and reproducible grading systems. Both grading systems consist of 3-point scales. See Figure 2 for our interpretation of the two grading systems. Kim et al. used an imaging software (ImageJ) for assessment of BAD, an objective, quantitative and reproducible method, however time-consuming and not easy to use in the everyday clinic (15). Dyrberg et al. presented the NSE grading scale, evaluating the degree of tissue distortion in these three areas of the breast by two plastic surgeons. They used video recordings for assessment of BAD, and found moderate (74%) to strong (88%) inter- and intraobserver agreements. Overall the grading system was rated simple, reproducible and useful for clinical use (14). The NSE grading scale, is qualitative and therefore more subjective than Kim et al.’s grading scale, however Kim et al.’s grading scale is more time-consuming for clinical use. Both studies were limited by the small sample sizes. Consistent with the findings of Kim et al., Cheffe et al. suggested a demarcation of topographic landmarks and linear segments between landmarks to quantify breast distortion (21). However, they did not define, how BAD could be assessed with this objective demarcation, thus the study was not included in this review. Furthermore, there were no statistically significant differences between the quantified demarcation and the degree of deformity. Further modifications are therefore needed for the use of Cheffe et al.’s method for quantifying the degree of BAD with a grading scale or numerical severity scale for either clinical or research purposes. As BAD has attained more attention in recent years, the use of standardized grading scales is needed for comparative research (8,25-28).
An optimal grading system is based on objectivity, reproducibility and applicability for every-day clinical use. However, a significant aspect of the grading systems is the patient-perception of BAD and the correlation between the clinically graded severity and the patient-perceived deformity (4,13,29). Six studies assessed patient-reported outcomes either for HR-QOL assessments or assessment of the patient’s evaluation of the degree of BAD (1,4,9,13,15,16). Four studies used a self-developed, however not validated questionnaires for assessing the degree of BAD (1,4,13,15). Despite the methodological limitation of the questionnaires, patients reported a prevalence of BAD between 25% to 75% and patients evaluated the degree of BAD higher than the clinical evaluations in three studies (4,13,15). Hence, more studies are needed where the patient’s perspective are included in the assessment of BAD using validated questionnaires. Two studies used the validated BREAST-Q for assessment of HR-QOL (9,16). Bracaglia et al. (2019) used BREAST-Q for assessment of the surgical techniques, and not to the degree of BAD (9). Fracol et al. (2020) however, correlated their quantitative grading system of BAD against BREAST-Q patient-reported outcomes. Surprisingly, their findings suggested that patients with increasing severity of animation deformity (grade 3) had better physical well-being scores, than grade 1 patients. Grade 3 patients had significantly less pulling, less nagging and less aching pain in the breast area compared to grade 1. Additionally, grade 1 patients had significantly higher rates of revision surgery than grade 2. Nonetheless, grade 3 patients had the highest number of revisional surgery than grade 1 and grade 2 patients (16). This finding is contradictory of other studies, where BAD was suggested to have a negative impact on HR-QOL (3-5). Correspondingly, a systematic review and meta-analysis found no difference of BREAST-Q scores for HR-QOL and satisfaction with the outcome in the prepectoral and subpectoral groups (28). However, Cattelani et al. showed significantly better psychosocial well-being and satisfaction with the outcome in the prepectoral group (30). While, Baker et al. compared short-term outcomes of subpectoral and prepctoral immediate breast reconstruction, and found significantly more patients in the prepectoral group, that reported more visible implant rippling than in the subpectoral group, and were overall more dissatisfied (31).
The disparity of varying reported rates of BAD is speculated to be due to numerous factors; (I) the subjectivity of current assessment scales, apart from NSE and Kim et al.’s grading system (14,15); (II) inconsistent categorization of mild to severe BAD, (III) the various surgical techniques used, (IV) the size and study types used for the assessment of BAD, and (V) the placement of the implant (sub- or prepectorally pocket). The subjectivity and inconsistency of grading scales may have resulted in over- and underestimation of BAD, depending on the grading system. The subjectivity is however minimized with the use of standardized, high-quality grading scales such as Kim et al. and the NSE grading scale (14,15) and more consistent categorization of the degree of BAD will be possible (8) in future studies.
We developed the NSE grading scale due to the limitation of existing grading systems. The interpretation of the NSE-grading scale has been further developed as the scores can be accumulated for a more consistent categorization of mild to severe BAD. The NSE grading scale scores from zero to two points in each of the three features (nipple, skin, and the entire breast) were 0 represents no visible distortion, 1 represents visible distortion, and 2 represents severe distortion, resulting in a total of zero to six points for all features. For more consistent categorization of BAD the summed scores of all features represents the severity of BAD; a total of 0–2 points represents mild BAD, 2–4 points represents moderate BAD, and 4–6 points represents severe BAD (14). This point accumulation for the degree of BAD was used for the calculation of the prevalence of BAD in the subpectoral implant placement group versus the prepectoral implant placement group (94.7% versus 10.5%). Surprisingly, we found the prevalence of BAD to be 10.5 percent in patients reconstructed using the prepectoral technique, which we had not expected. However, the number of high-quality studies reporting BAD is scarce and future studies will show if the prevalence is true. Dyrberg et al. is to our knowledge the first study using a high-quality grading scale to evaluate both subpectoral and prepectoral implant pocket placements in relation to BAD (14).
The evidence is conflicting regarding the various surgical techniques and the impact on the degree of BAD (5,26-28,32-35). Most studies have assessed subpectoral implant placement when assessing BAD (1,9,11-13,16,36). In our previous review, we postulated, that the degree of muscle involvement in the breast reconstruction may be proportional with the degree of BAD, as the Regnault technique had the highest prevalence of severe BAD (12). A meta-analysis was not possible to conduct, as most studies assessed subpectoral implant placement (and the various techniques used in subpectoral plane) and only one study assessed prepectoral implant placement. Nonetheless, a total of 2 patients had some degree of BAD in the prepectoral group out of 19 patients, while 1345 patients had some degree of BAD in the subpectoral group out of 1819 patients. The prevalence of BAD was significantly higher in the subpectoral group compared to the prepectoral group with a relative risk (RR) of 0.14, 95% CI: 0.04–0.53; P value <0.004. This study is to our knowledge the first to quantify the prevalence of BAD in relation to implant pocket placement. In a meta-analysis Li et al. compared prepectoral to subpectoral implant-based reconstruction regarding various outcomes (capsular contraction, quality of life, pain, skin necrosis, and implant loss), however they found no cases of BAD and therefore could not conduct an analysis of BAD regarding implant placement (10). Yang et al. found a prevalence of BAD on 8.5% in the subpectoral group versus 0% in the prepectoral group (37), they however did not define, how BAD was graded. We found a significantly higher prevalence of BAD in both the subpectoral and prepectoral group, however, the findings of Yang et al. were consisting to our findings regarding higher prevalence of BAD in subpectoral implant placement compared to prepectoral implant placement.
Subpectoral implant placement has been the gold standard of breast reconstruction for more than five decades (32). Several studies have recently suggested correction of BAD by converting the implant from a subpectoral plane to a prepectoral placement, particularly with the use of ADM (5,25-27,32-35,38). It is theorized that repositioning of the implant to a prepectoral plane separates the contracting muscle from the overlying skin and thereby reversing the animation deformity (5,25,39). Hammond et al. described a 100% resolution of BAD by changing to a prepectoral plane in 19 breasts (35). The etiology of BAD, the impact of surgical techniques, and implant placement may not be as simple, as described in previous studies. In this review, we have shown that prepectoral implant placement has significantly lower prevalence of BAD, however prepectoral implant did not result in complete elimination of BAD with a prevalence of 10.5%. A simple change from a subpectoral to prepectoral plane may therefore not solve the BAD-related problems. The degree of BAD in patients reconstructed by partial submuscular technique may differ between those reconstructed with or without mesh/ADM. However, the limited number of high-quality studies reporting on BAD does not allow for subgroup analysis between partial sub-muscular reconstruction with or without the use of mesh/ADM. (5,25,32,33).
Prepectoral implant placement may provide more natural aesthetic results, reduce postoperative pain, and shortens the recovery period (27,40). Prepectoral implant placement is associated with a higher incidence of capsular contracture (41). However, we do not know if the associated higher incidence of encapsulation is true after the introduction of ADM. In addition, prepectoral breast reconstruction requires the mastectomy/reconstructive flaps to be of sufficient thickness and vitality and it increases the risk of rippling and implant edge visibility (22,37). Subpectoral implant placement has lower rates of capsular contraction and flap thickness is not as crucial as in prepectoral implant placement (29,37,41). Although the prevalence of BAD is higher in the subpectoral group compared to the prepectoral group in this review, the studies have significant limitations with insufficient number of patients, the use of non-standardized grading systems, and only three studies assessing prepectoral implant placement (14,22,37). The evidence is insufficient to advocate one implant pocket placement over another with the existing literature. We can merely advocate for a more comprehensive and individualized selection of implant plane depending on patients/breasts (29,42), as limited studies have examined the differences of implant pocked placement and surgical technique on BAD with the use of standardized and high-quality grading systems (1,9,11-16,18,20,22,37).
There are some limitations in this review. A meta-analysis was not conducted, as the methods of assessing BAD were not comparable, due to variations from 4-point scales to 3-point scales, from surgeon to patient-self assessment, and variation of type of surgery. Only one retrospective study compared the two implant pocket planes, and the study was limited by a small sample size. However, BAD was assessed with the use of the high-quality NSE grading scale (14). Further limitations are that only retrospective-, prospective studies and reviews were included in this review, as no RCT studies have been published assessing BAD. Various surgical techniques and pocket implant placements were presented in breast reconstruction and augmentation (1,11-15,18). However, only few comparative studies were available with clear description of study design, participants and standardized grading systems (1,14-16). The sample sizes of the included studies were small, with only two larger studies comprising of 580 and 605 patients (9,12). Large, multicenter, randomized-controlled trials are needed for further evaluation of the etiology and prevalence of BAD with the use of standardized grading systems.
Conclusions
This systematic review is the newest update on the various BAD grading systems available, and the quality and reproducibility of the individual grading systems. We recommend two grading systems, the qualitative NSE grading scale and Kim et al.’s quantitative grading system—two high quality, reproducible and clinically-relevant assessment methods. Patients with prepectoral implant placement have a significantly lower prevalence of BAD compared to patients with subpectoral implant placement (10.5% versus 73.9%). The total prevalence of some degree of BAD was 73.3% regardless of implant placement and surgical techniques. The evidence is still inadequate in the existing studies and more studies, especially randomized-controlled trials are needed were these reliable and high-quality grading systems are used in combination of validated patient-reported outcome measures to further investigate and understand the etiology of BAD.
Acknowledgments
The authors are very grateful to MD Maiken Bjerregaard for her assistance with designing the illustration of the two recommended grading systems.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Breast Surgery for the series “Breast Reconstruction - The True Multidisciplinary Approach”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://abs.amegroups.com/article/view/10.21037/abs-21-46/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://abs.amegroups.com/article/view/10.21037/abs-21-46/coif). The series “Breast Reconstruction - The True Multidisciplinary Approach” was commissioned by the editorial office without any funding or sponsorship. JT served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Breast Surgery from December 2019 to November 2023. CB serves as the unpaid editorial board members in Annals of Breast Surgery from August 2019 to July 2023. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Spear SL, Schwartz J, Dayan JH, et al. Outcome assessment of breast distortion following submuscular breast augmentation. Aesthetic Plast Surg 2009;33:44-8. [Crossref] [PubMed]
- Alnaif N, Safran T, Viezel-Mathieu A, et al. Treatment of breast animation deformity: A systematic review. J Plast Reconstr Aesthet Surg 2019;72:781-8. [Crossref] [PubMed]
- Strasser EJ. Results of subglandular versus subpectoral augmentation over time: one surgeon's observations. Aesthet Surg J 2006;26:45-50. [Crossref] [PubMed]
- Becker H, Fregosi N. The Impact of Animation Deformity on Quality of Life in Post-Mastectomy Reconstruction Patients. Aesthet Surg J 2017;37:531-6. [Crossref] [PubMed]
- Gabriel A, Sigalove S, Sigalove NM, et al. Prepectoral Revision Breast Reconstruction for Treatment of Implant-Associated Animation Deformity: A Review of 102 Reconstructions. Aesthet Surg J 2018;38:519-26. [Crossref] [PubMed]
- Reitsamer R, Peintinger F. Prepectoral implant placement and complete coverage with porcine acellular dermal matrix: a new technique for direct-to-implant breast reconstruction after nipple-sparing mastectomy. J Plast Reconstr Aesthet Surg 2015;68:162-7. [Crossref] [PubMed]
- Wallace MS, Wallace AM, Lee J, et al. Pain after breast surgery: a survey of 282 women. Pain 1996;66:195-205. [Crossref] [PubMed]
- Dyrberg DL, Bille C, Gunnarsson GL, et al. Breast animation deformity. Arch Plast Surg 2019;46:7-15. [Crossref] [PubMed]
- Bracaglia R, Servillo M, Fortunato R, et al. The Triple Plane, the Bra-Flap, and the Inverted Bra-Flap Modified Dual Plane Techniques for Breast Augmentation. Aesthet Surg J 2020;40:NP141-51. [Crossref] [PubMed]
- Li Y, Xu G, Yu N, et al. Prepectoral Versus Subpectoral Implant-Based Breast Reconstruction: A Meta-analysis. Ann Plast Surg 2020;85:437-47. [Crossref] [PubMed]
- Bracaglia R, Tambasco D, Gentileschi S, et al. Triple-plane technique for breast augmentation: solving animation deformities. Aesthetic Plast Surg 2013;37:715-8. [Crossref] [PubMed]
- Pelle-Ceravolo M, Del Vescovo A, Bertozzi E, et al. A technique to decrease breast shape deformity during muscle contraction in submuscular augmentation mammaplasty. Aesthetic Plast Surg 2004;28:288-94. [Crossref] [PubMed]
- Nigro LC, Blanchet NP. Animation Deformity in Postmastectomy Implant-Based Reconstruction. Plast Reconstr Surg Glob Open 2017;5:e1407. [Crossref] [PubMed]
- Dyrberg DL, Gunnarsson GL, Bille C, et al. A simple clinical assessment of breast animation deformity following direct-to-implant breast reconstruction. Arch Plast Surg 2019;46:535-43. [Crossref] [PubMed]
- Kim JYS, Qiu CS, Chiu WK, et al. A Quantitative Analysis of Animation Deformity in Prosthetic Breast Reconstruction. Plast Reconstr Surg 2019;144:291-301. [Crossref] [PubMed]
- Fracol M, Qiu CS, Chiu MW, et al. The Relationship between Animation Deformity and Patient-Reported Outcomes: Application of the BREAST-Q to a Quantitative Stratification of Animation Severity. Plast Reconstr Surg 2020;145:11-7. [Crossref] [PubMed]
- Kümmel S, Kümmel A, Hagemann F, et al. Jumping Breast Phenomenon Following Subcutaneous Mastectomy: First Description and Grading of a Well-Known Breast Deformity. Breast Care (Basel) 2018;13:354-8. [Crossref] [PubMed]
- Vidya R, Tafazal H, Salem F, et al. Management based on grading of animation deformity following implant-based subpectoral breast reconstruction. Arch Plast Surg 2018;45:185-90. [Crossref] [PubMed]
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [Crossref] [PubMed]
- Fracol M, Feld LN, Chiu WK, et al. An overview of animation deformity in prosthetic breast reconstruction. Gland Surg 2019;8:95-101. [Crossref] [PubMed]
- Cheffe MR, Valentini JD, Collares MVM, et al. Quantifying Dynamic Deformity After Dual Plane Breast Augmentation. Aesthetic Plast Surg 2018;42:716-24. [Crossref] [PubMed]
- Vidya R, Iqbal FM, Becker H, et al. Rippling Associated with Pre-Pectoral Implant Based Breast Reconstruction: A New Grading System. World J Plast Surg 2019;8:311-5. [PubMed]
- Gunnarsson GL, Thomsen JB. Prepectoral Hammock and Direct-to-implant Breast Reconstruction in 10 Minutes: A Focus on Technique. Plast Reconstr Surg Glob Open 2018;6:e1931. [Crossref] [PubMed]
- Dyrberg DL, Bille C, Gunnarsson GL, et al. Visualized pre- and subpectoral implant placement for immediate breast reconstruction. Gland Surg 2019;8:S251-4. [Crossref] [PubMed]
- Lentz R, Alcon A, Sbitany H. Correction of animation deformity with subpectoral to prepectoral implant exchange. Gland Surg 2019;8:75-81. [Crossref] [PubMed]
- Ribuffo D, Berna G, De Vita R, et al. Dual-Plane Retro-pectoral Versus Pre-pectoral DTI Breast Reconstruction: An Italian Multicenter Experience. Aesthetic Plast Surg 2021;45:51-60. [Crossref] [PubMed]
- Sbitany H, Piper M, Lentz R. Prepectoral Breast Reconstruction: A Safe Alternative to Submuscular Prosthetic Reconstruction following Nipple-Sparing Mastectomy. Plast Reconstr Surg 2017;140:432-43. [Crossref] [PubMed]
- Li L, Su Y, Xiu B, et al. Comparison of prepectoral and subpectoral breast reconstruction after mastectomies: A systematic review and meta analysis. Eur J Surg Oncol 2019;45:1542-50. [Crossref] [PubMed]
- Li S, Mu D, Liu C, et al. Complications Following Subpectoral Versus Prepectoral Breast Augmentation: A Meta-analysis. Aesthetic Plast Surg 2019;43:890-8. [Crossref] [PubMed]
- Cattelani L, Polotto S, Arcuri MF, et al. One-Step Prepectoral Breast Reconstruction With Dermal Matrix-Covered Implant Compared to Submuscular Implantation: Functional and Cost Evaluation. Clin Breast Cancer 2018;18:e703-11. [Crossref] [PubMed]
- Baker BG, Irri R, MacCallum V, et al. A Prospective Comparison of Short-Term Outcomes of Subpectoral and Prepectoral Strattice-Based Immediate Breast Reconstruction. Plast Reconstr Surg 2018;141:1077-84. [Crossref] [PubMed]
- Jones GE, King VA, Yoo A. Prepectoral Site Conversion for Animation Deformity. Plast Reconstr Surg Glob Open 2019;7:e2301. [Crossref] [PubMed]
- Kobraei EM, Cauley R, Gadd M, et al. Avoiding Breast Animation Deformity with Pectoralis-Sparing Subcutaneous Direct-to-Implant Breast Reconstruction. Plast Reconstr Surg Glob Open 2016;4:e708. [Crossref] [PubMed]
- Khan UD. Dynamic breasts: a common complication following partial submuscular augmentation and its correction using the muscle-splitting biplane technique. Aesthetic Plast Surg 2009;33:353-60. [Crossref] [PubMed]
- Hammond DC, Schmitt WP, O'Connor EA. Treatment of breast animation deformity in implant-based reconstruction with pocket change to the subcutaneous position. Plast Reconstr Surg 2015;135:1540-4. [Crossref] [PubMed]
- Pantelides NM, Srinivasan JR. Rippling Following Breast Augmentation or Reconstruction: Aetiology, Emerging Treatment Options and a Novel Classification of Severity. Aesthetic Plast Surg 2018;42:980-5. [Crossref] [PubMed]
- Yang JY, Kim CW, Lee JW, et al. Considerations for patient selection: Prepectoral versus subpectoral implant-based breast reconstruction. Arch Plast Surg 2019;46:550-7. [Crossref] [PubMed]
- Holland MC, Lentz R, Sbitany H. Surgical Correction of Breast Animation Deformity with Implant Pocket Conversion to a Prepectoral Plane. Plast Reconstr Surg 2020;145:632-42. [Crossref] [PubMed]
- Jones G, Antony AK. Single stage, direct to implant pre-pectoral breast reconstruction. Gland Surg 2019;8:53-60. [Crossref] [PubMed]
- Snyderman RK, Guthrie RH. Reconstruction of the female breast following radical mastectomy. Plast Reconstr Surg 1971;47:565-7. [Crossref] [PubMed]
- Egeberg A, Sørensen JA. The Impact of Breast Implant Location on the Risk of Capsular Contraction. Ann Plast Surg 2016;77:255-9. [Crossref] [PubMed]
- Hunstad JP, Webb LS. Subfascial breast augmentation: a comprehensive experience. Aesthetic Plast Surg 2010;34:365-73. [Crossref] [PubMed]
Cite this article as: Dalaei F, Dyrberg DL, Bille C, Salzberg CA, Sørensen JA, Thomsen JB. An update on breast animation deformity grading systems—a systematic review. Ann Breast Surg 2022;6:26.