Identification of factors that predict premature tissue expander loss in immediate breast reconstruction
Introduction
Between 65–75% of breast reconstructions in the U.S. employ tissue expander (TE) and implant-based reconstruction (1). This method provides practical advantages including shorter operative time and faster recovery (1,2). Despite these advantages, there are still pitfalls to TE-based reconstruction. The overall prevalence of TE failure is unclear since this varies by institution, patient population, follow-up period. One of the largest analyses of premature TE loss looked at 14,585 patients from a national database over a 5-year period and found that 119 patients lost their expander, or 0.8% of the study population; however, this study only had a 30-day follow-up period (2). There are various, well-established risk factors that predispose patients to TE loss before successful completion of expansion. Obesity, smoking, hypertension, wound infection, older age, and prior radiation to the breast have been significantly associated with an increased risk of complications in expander-based reconstruction by several sources (1-7).
Determining the risk factors that may predispose patients to premature, unplanned TE loss is essential for several reasons. First, breast cancer patients undergoing mastectomy experience not only massive physical changes that exhaust their bodies, but also emotional changes that may have a negative effect on their mental well-being, body image, sexuality, and self-esteem. Minimizing reoperation is essential for protecting the integrity of patients’ physical and psychological health. Second, reoperations and the complications that beget them are associated with higher cost. Yan et al. showed that unplanned readmissions or reoperations also significantly increased total cost (7). Expander reconstruction complicated by infection or prosthetic exposure—two events that usually require reoperation—increased costs by $12,554 and $17,153 respectively (7).
The purpose of this study was to identify potential predictors of premature, unplanned TE loss in immediate breast reconstruction. Prior studies have included larger numbers of patients, those studies were also extremely varied in the composition of their study population, methods of reconstruction, institutional policies, and also focus more on complications associated with breast reconstruction (2-6). While this study is smaller than these prior studies, this study had less variability between groups by utilizing relatively similar patient populations who accessed care at the same urban, academic medical center. There were four surgeons, all of whom used the same product brands and had similar criteria for use of acellular dermal matrix (ADM). During the timeframe of this study, all expanders were placed in a submuscular position. All patients were cared for by the same team, and all were seen at the same two outpatient sites postoperatively. This allows for a more accurate comparison due to minimal differences in patient care standards, and thus a better ability to draw conclusions about the implications of any findings on patient care.
We hypothesized that the findings of our study would be consistent with prior studies—particularly body mass index (BMI), age, smoking status, and prior radiation status. Additionally, we postulated that race and socioeconomic status would have an impact on TE loss. Socioeconomic status and race have been shown to influence a patient’s decision to undergo breast reconstruction because of a perceived lack of education provided by the clinician (8). There is also evidence of a survival benefit in breast reconstruction patients with higher income and insurance (9).
We also hypothesized that drain duration and total expander capacity would be associated with BMI, and thus would also have an association with TE loss. Negative suction drainage is important for reducing seroma and hematoma formation by minimizing dead space created during surgery. Use of drains in obese patients undergoing abdominal surgery has been shown to have more drainage, require longer drain duration, and have better wound healing (10,11). Larger breast mass and BMI has also been associated with longer drain duration and more drainage in patients undergoing expander-based reconstruction (12). However, longer drain duration has also been shown to be independently associated with increased infection rates after immediate breast reconstruction (13). One study postulated that early removal may mitigate the retrograde migration of bacteria and decrease risk of infection (13). Thus, we anticipated that a longer placement of drains would occur in obese patients which may predispose to infection – the most common reason for TE loss.
Additionally, patients with larger breasts generally require larger TE due to having a larger breast pocket (14). Francis et al. and Khansa et al. have shown that larger cup size is associated with increased risk for infection (15,16). Larger breast width has also been shown in the literature to be associated with increased rates of seroma, cellulitis, and skin necrosis (12). The width of the expander base is typically how women are fit for appropriate expander size, and therefore, we hypothesized that this association between breast size, BMI, and infection would also be significantly associated with TE loss. Our goal in completing this study was to identify which risk factors, if any, may be associated with premature expander loss in order to better stratify the risk for TE-based reconstruction failure so that breast cancer patients can make the most informed decision regarding their breast reconstruction. We present the following article in accordance with the STROBE reporting checklist (available at https://abs.amegroups.com/article/view/10.21037/abs-21-77/rc).
Methods
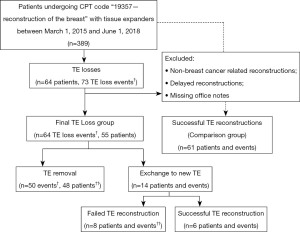
A total of 389 patients undergoing any procedure classified by Current Procedural Terminology (CPT) code “19357—tissue expander placement in breast reconstruction, including subsequent expansion(s)” between March 2015 and June 2018 at a single, urban institution were identified by electronic medical record search. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional review board of Cooper University Health Care (ID: 18-162) and individual consent for this retrospective analysis was waived. Charts were reviewed and 64 patients (TE Loss group) were identified who had TE loss prior to completion of reconstruction. Any patients who had non-breast cancer related reconstructions, delayed reconstruction, or whose case predated the use of the electronic medical record were then excluded, leaving 55 TE loss patients experiencing 64 TE loss events.
TE loss events outnumbered patients due to the bilaterality of most reconstructions. Patients undergoing delayed reconstruction with TE were excluded in order to have the most homogeneous study group possible. Potential differences in the two groups due to differences in operative time, potential for hematoma and seroma, potential for skin necrosis, and effect of scarring were felt to be possible confounding factors that might make immediate and delayed reconstructions dissimilar. For these reasons, we chose to look only at immediate reconstructions. Patients were followed from initial mastectomy and insertion of expanders until loss or successful reconstruction. Breast cancer gene (BRCA)-positive patients undergoing prophylactic mastectomy and reconstruction were included in analysis. Patients with missing variable data points—for example, their BMI was not documented—were not included in statistical analysis for that specific variable.
The remaining master list of patients was then randomized, and the charts examined sequentially using the same exclusion criteria to obtain a similar sized comparison group that was large enough for statistical analysis. Sixty-one successfully reconstructed patients were included in that group (Comparison group). The process for patient selection is summarized in Figure 1.
Patient characteristics, intraoperative, and postoperative factors were collected for analysis (Table 1). Since socioeconomic status may be linked to poorer outcomes, we attempted to investigate this variable. As individual income data were not available, patient zip codes were collected and categorized according to United States Census Bureau income statistics in order to determine median and mean income, and resultingly socioeconomic status, for each group. It is also important to note that characterization of the reason for expander loss was complex given the interconnected nature of wound breakdown and infection. Patients classified as “infection only” had no evidence of wound breakdown or loss of skin integrity but showed clinical signs of infection such as fever or erythema and pain. Those classified “wound problem only” had dehiscence or other wound issues without clinical evidence of infection. Patients classified as “wound problem and infection” fell into both categories. Patients whose expanders ruptured or had a filling defect due to a leak were classified as loss due to “mechanical issues”.
Table 1
| Patient characteristics |
| Age |
| Race |
| Socioeconomic statusϯ |
| Body mass index |
| Immunocompromised status |
| Diabetes |
| Smoking status |
| Neoadjuvant or adjuvant chemotherapy |
| Radiation status |
| Cancer laterality |
| Cancer stage |
| Prophylactic status |
| Reasons for expander loss |
| Infection only |
| Wound problem + infection |
| Wound problem only |
| Mechanical failure |
| Other |
| Surgical factors |
| Operative time |
| Surgical laterality |
| Expander capacity |
| Intraoperative expander fill |
| Type of mastectomy |
| Type of incision |
| Use of acellular dermal matrix |
| Nodal surgery |
| Axillary drains |
| Breast drains |
| Duration of drains |
| Skin necrosis |
| Seroma occurrence and volume |
| Final expander fill volume |
| Number of postoperative visits |
| Number of postoperative readmissions |
| Character of postoperative readmissions |
ϯ, U.S. census data was employed to determine median and mean income for a patient’s zip code as a proxy for socioeconomic status.
All surgeries were performed in the same hospital, utilizing the same care team. Four plastic surgeons performed the reconstructions. Patients were distributed to the surgeons by availability, and in some cases, by specific patient or oncologic surgeon request. During the course of this study, all reconstructions were subpectoral. All patients were admitted for at least 23 hours, and length of stay was based on clinical need or patient preference. All patients had breast drains placed. Patients received either single dose or less than 24-hour prophylactic antibiotics, which was cefazolin or either clindamycin or vancomycin for penicillin-allergic patients. Drains were removed based on drain output levels.
Patients who developed signs of superficial surgical site infection (redness and tenderness) were given a trial of trimethoprim/sulfamethoxazole if mild, or intravenous vancomycin if more significant. Patients who showed signs of sepsis, who had purulent drainage or aspirate, or who declined a trial of antibiotic therapy underwent removal of their expanders. Shared decision making was used for removal of a contralateral uninfected expander with some patients electing to have both removed.
Statistical analysis
TE Loss and Comparison groups were compared using Fisher’s exact test for categorical variables and t-test for continuous variables. Single variable predictors of TE and Wise incision were analyzed using univariate logistic regression. Odds ratios (ORs) with 95% confidence intervals were derived for each predictor of TE loss. A Youden’s J test was performed to determine a cut-off point at which an association between these variables, if it existed, may be significant. This value was determined to be a BMI of 23 kg/m2 because this was the most sensitive and specific point (sensitivity =42.6%, specificity =89.8%).
Results
Of the final TE Loss group of 55 patients and 64 TE loss events, 50 of these events proceeded to permanent TE removals while 14 events were TE exchanges. This accounted for 48 patients having eventual permanent TE removal and 14 patients having exchanges. Patients who underwent exchange that was unsuccessful and led to expander removal were counted as two separate events, and their removal event was subsequently included in the TE Loss group. The average time to loss was 63.92 days. Patients who lost their expander were offered reconstructive alternatives appropriate to their individual case, and shared decision making was employed to find the best solution. The majority of these patients elected to forego reconstruction. Exchange rather than removal was performed most often due to loss for mechanical issues with the expander. In instances of loss due to wound breakdown, selected low infection risk patients were offered the option of exchange rather than removal. Patients were considered to be low infection risk based on clinical exam, and this was consistent among authors. Examples of patients who fit this category included those with skin flap necrosis without implant exposure, excessive drain output without purulence, and wound drainage with pinpoint dehiscence of <24 hours duration without erythema, fever, or purulence. Patients with mechanical complications such as expander rupture were also offered exchange. Of the 14 TE exchanges, 6 completed reconstruction (43% successful salvage). In the successful salvage group, three patients had their expanders exchanged for mechanical issues, two for wound breakdown and infection, and one for a wound issue only. Five patients in the Comparison group and 11 patients in the TE Loss group underwent prophylactic mastectomy. Having a prophylactic mastectomy was not significantly associated with TE loss (P=0.1407).
TE Loss and Comparison groups were relatively similar. Patient characteristics are shown in Table 2. The number of patients missing data for each variable is shown in Table 3. The most common reason for premature expander loss was infection with 38% of TE losses occurring for this reason (n=24 events, 24 patients). Twenty-eight percent of patients had their TE removed for wound problem and infection (n=18 events, 17 patients), 20% for wound problem only (n=13 events, 12 patients), and 11% for mechanical failure (n=7 events, 6 patients). Only two patients (representing two events) comprising 3% of the study population fell into the “other” category—one was removed without known problems by patient choice and the other was removed for concerning radiation changes to the area with patient choice to abandon reconstruction.
Table 2
| Patient characteristics | Comparison group | TE Loss group | OR (95% CI) | P value |
|---|---|---|---|---|
| Age (years), mean ± SD | 50.98±10.20 | 56.74±10.10 | 1.058 (1.019, 1.098) | 0.03 |
| Race, n (%) | ||||
| Asianϯ | 2 (3.3) | 0 (0.0) | 4.895 (0.229, 104.724) | 0.50 |
| Blackϯ | 6 (10.0) | 10 (15.6) | 1.703 (0.572, 5.068) | 0.34 |
| Hispanicϯ | 5 (8.3) | 8 (12.5) | 1.635 (0.498, 5.368) | 0.42 |
| Whiteϯ | 47 (78.3) | 46 (71.9) | – | |
| BMI (kg/m2), mean ± SD | 26.2±4.6 | 29.8±8.7 | 1.083 (1.021, 1.148) | 0.08 |
| Income (USD), mean ± SD | 85,070±25,909 | 81,049±26,177 | 0.941 (0.820, 1.081) | 0.39 |
| Income (USD), median ± SD | 70,812±20,766 | 67,917±22,134 | 0.938 (0.794, 1.108) | 0.45 |
| Smoking status, n (%) | 1.811 (0.897, 3.658) | 0.09 | ||
| Never smoker | 50 (82.0) | 48 (75.0) | – | |
| Former smoker | 0 (0.0) | 6 (9.4) | – | |
| Current smoker | 11 (18.0) | 10 (15.6) | – | |
| Immunocompromised status, n (%) | 1 (1.6) | 4 (6.3) | 4.000 (0.434, 36.840) | 0.22 |
| Diabetes mellitus status, n (%) | 4 (6.6) | 11 (17.2) | 2.958 (0.887, 9.858) | 0.08 |
| Neoadjuvant chemotherapy, n (%) | 16 (26.2) | 19 (29.7) | 1.187 (0.543, 2.598) | 0.67 |
| Adjuvant chemotherapy, n (%) | 14 (23.0) | 11 (17.2) | 0.697 (0.288, 1.683) | 0.42 |
| Postmastectomy radiation, n (%) | 14 (23.0) | 18 (28.1) | 1.314 (0.585, 2.947) | 0.51 |
| Cancer stage, clinical, n (%) | 1.187 (0.833, 1.691) | 0.35 | ||
| Stage 0 (DCIS) | 17 (30.9) | 13 (24.5) | ||
| Stage 1 | 19 (34.5) | 16 (30.2) | ||
| Stage 2 | 12 (21.8) | 14 (26.4) | ||
| Stage 3 | 5 (9.1) | 10 (18.9) | ||
| Stage 4 | 2 (3.6) | 0 (0.0) | ||
| Prophylactic mastectomy, n (%) | 5 (8.2) | 11 (17.2) | 2.324 (0.757, 7.135) | 0.14 |
ϯ, White race was used as a comparison point for other racial groups in terms of the likelihood of losing expander. OR, odds ratio; CI, confidence interval; SD, standard deviation; BMI, body mass index; TE, tissue expander; DCIS, ductal carcinoma in situ.
Table 3
| Variables | Comparison group (%) | TE Loss group (%) |
|---|---|---|
| Race | 1.6 | – |
| BMI | 3.3 | 6.3 |
| Cancer laterality | 9.8ϯ | 20.8ϯϯ |
| Cancer stage | 9.8ϯ | 20.8ϯϯ |
| Intraoperative fill volume | 3.2 | 12.5 |
| Type of Mastectomy | 3.2 | – |
| Incision type | 3.2 | 10.4 |
| Acellular dermal matrix (ADM) use | – | 2.1 |
| Drain duration | 8.2 | 52.0 |
| Final fill volume | 1.6 | 4.0 |
ϯ, four of these patients had prophylactic mastectomy; ϯϯ, nine of these patients had prophylactic mastectomy. TE, tissue expander; BMI, body mass index; ADM, acellular dermal matrix.
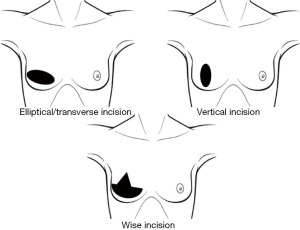
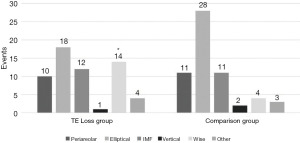
Older age, elevated BMI, and use of the Wise pattern incision were found to be associated with increased risk of expander loss. On average, the TE Loss group was older than the Comparison group. This difference was statistically significant with a 5.8% increased risk of TE loss with each year of age (OR =1.058, P=0.03). There was a significant relationship between BMI and risk of TE loss. For each unit increase in BMI, there was an 8.3% increased risk of TE loss (OR =1.083, P=0.08). Within both groups, elliptical incisions represented the majority performed (Figures 2,3). Patients with a Wise pattern incision had a 6.65-time greater risk of TE loss, and this was statistically significant (OR =1.066, P=0.0002). Furthermore, BMI was a significant predictor of Wise incision. For each unit increase of BMI, there was a 16.64% increase in the chance of having a Wise incision (P<0.05).
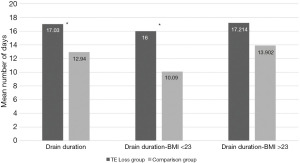
The TE Loss group had their drains in for approximately four days longer on average than the Comparison group, and this longer duration of drain placement was also a significant predictor of TE loss (OR =1.078, P=0.018) (Figure 4). Duration of drain placement was also significantly associated with BMI. Drain duration increased the risk for TE loss 46.9% per day when BMI was less than 23 kg/m2 (OR =1.469, P=0.0063). When BMI was greater than 23 kg/m2, drain duration was not a significant risk factor for TE loss (P=0.123).
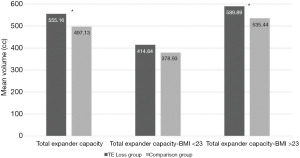
A larger expander fill capacity was the final significant predictor of TE loss (OR =1.003, P=0.017) (Figure 5). The TE Loss and Comparison groups had an average expander fill capacity of 555.16 cc [standard deviation (SD) =142.29 cc] and 497.13 cc (SD =117.46 cc) respectively. Larger total expander capacity increased the risk for TE loss 50.9% per 100 cc when BMI was greater than 23 kg/m2 (OR =1.51, P=0.0316). TE volume was not a significant risk factor for TE loss when BMI was less than 23 kg/m2 (P=0.107).
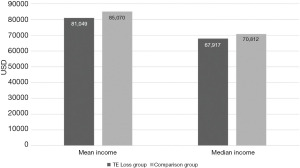
Socioeconomic status, represented by the median and mean income within each patient’s zip code, was not a significant factor in predicting premature TE loss (mean OR =0.941, P=0.39; median OR =0.938, P=0.45) (Figure 6). Race, which is often strongly associated with socioeconomic status, was not a statistically significant predictor of TE loss (P=0.3611).
A diagnosis of diabetes mellitus was not associated with premature TE loss (P=0.08). Immunocompromised conditions, i.e., a history of splenectomy, were not associated with premature TE loss (P=0.22). Post-mastectomy radiation treatment did not increase the risk of premature TE loss (P=0.54). No other demographic, intraoperative, or postoperative factor analyzed in this study was associated with premature TE loss.
Discussion
In this study, age, BMI, drain duration, total expander capacity, and Wise incision were risk factors for premature TE loss. However, the effects of drain duration, total capacity, and Wise incision are also significantly associated with BMI. Use of the Wise incision pattern can improve shape in the reconstruction of the large breast. Obese patients tend to have larger breasts that benefit from use of the Wise pattern (17). Patients in our study with Wise incision were more likely to lose their expander as well as have a higher BMI. In this study, Wise incision had a significant association with both BMI and risk for TE loss separately, but a larger sample size of patients with Wise incisions, particularly those with normal BMI, would be necessary to determine if the incision pattern alone is an independent risk factor. The risk of losing an expander prematurely is also significantly associated with larger total expander capacity in more obese patients. Patients with larger BMIs typically have larger breasts and thus require larger expanders (12,15,16).
Longer drain duration did not have an effect on TE loss in patients with a larger BMI; it did, however, in patients with BMI <23 kg/m2. It would be expected that patients with a larger body habitus have their drains in longer because they usually have more drainage. While there is no association between drain duration and higher BMI in this study, it is important to note that drain duration itself is an independent risk factor for TE loss in this study. Longer drain duration has been associated with increased risk of infection in prosthesis-based reconstruction in the literature (18,19). It is not clear if this is due to the presence of the drain itself or due to the opportunity for ingress of microorganisms through the drain site or the collection bulb. Alternatively, a longer duration of drainage could indicate subclinical infection, increased lymphatic flow, or inflammation which then might be associated with overt infection. Our finding that longer drain duration in lower BMI patients, who otherwise might be expected to have less drainage, might lend support to this hypothesis.
To our knowledge, no other study has looked at socioeconomic status as a potential predictor for unplanned TE loss. Several studies have looked at the effect of race and socioeconomic differences on other parameters of breast reconstruction such as rate and type of reconstruction (8,9,20,21). Health disparities and access to care are major issues within our healthcare system, particularly with respect to complications and poor outcomes. While it may seem that there was no significant effect of race or socioeconomic status on premature TE loss in this study, both TE Loss and Comparison groups had median and mean income above the average household income in the United States. This indicates that despite being in an urban setting, the patients undergoing breast reconstruction at our institution, on average, may have had a higher socioeconomic status. However, our patient population does have a lower median income than that of our state as a whole. Using zip code and census data as a proxy for socioeconomic status may not accurately reflect an individual’s financial status which may vary widely within a zip code.
A study of over 600,000 women with breast cancer at various stages showed that most low income and uninsured patients did not receive reconstruction at all, and the opposite was true for those with high income and insurance (9). Patients in that study were also shown to present at a later stage of disease and were less likely to receive immediate breast reconstruction (9). In another study, a common trend among women making <$25,000/year, who were Hispanic, or whose highest level of education was a high school diploma was that not having enough information was the primary reason for not electing to undergo breast reconstruction (8). While low socioeconomic status and minority race were not significantly associated with TE loss in our study, it is important for surgeons to provide adequate information to these patients and counsel them on their historically higher risk for adverse outcomes.
There were other limitations of our study. The sample size was small and consisted only of 126 patients total, with only 64 TE losses representing 55 patients over a 3-year period. The majority of tissue-expander based reconstructions are successful. Exact loss rates vary by institution, country, patient volume and demographics, and follow-up period. A study by Cordeiro and McCarthy in 2008 looked at 1,221 patients up to a year after implant-based breasts reconstruction and determined a complication rate of 5.8% and a loss rate of 2.8% (22). Similarly, Fischer in 2013 looked at 14,585 patients from a national database and identified a loss rate of 0.8% at 30-days post-reconstruction (2). While the loss rate at our institution was larger at 16.45%, it is important to note that our follow-up period went beyond the 90-day global period, ending at the point at which the expander was lost for the TE Loss group or the permanent implant was placed for the Comparison group. A relatively higher loss rate is not unique to this study. Ota et al. 2016 had a loss rate of 15.5% (6). Our small study size had higher socioeconomic status than the national average and more white patients. We are at an urban institution and follow all the same practices, and surgical practices vary by institution. Furthermore, this study followed all patients to either successful expander or TE loss/exchange. The average time to loss was 63 days, indicating that it is common to have complications outside of the standard 30-day postoperative period. Meaningful comparison of studies with different endpoints is difficult. There is great variability in timing of expansion and expander to implant exchange, and we would propose that following to success or failure is more meaningful than a set time period. These aforementioned factors affect the external validity of our results.
A lack of consistency among patient records was an additional limitation of our study. Not all patients had a fully complete record with all of the information available. A significant portion of the TE Loss group (52%) was missing information about drain duration. Several patients were missing information in their record about the type of incision used for their mastectomy.
BMI may be the strongest risk factor established thus far for tissue-expander complications in breast reconstruction. It is ubiquitous in the literature as a risk factor for TE loss and complications, and it seems to have many effects on other parameters of the breast reconstruction process such as infection risk and incision type. Patient BMI should be an important factor in the decision-making process for immediate breast reconstruction. Obese patients should be counseled that their body habitus may predispose them to complications that could render this method of reconstruction unsuccessful, and they should be provided with alternatives to immediate, TE-based reconstruction.
Conclusions
In summation, age, BMI, drain duration, total expander capacity, and Wise incision were independent risk factors for premature, unplanned TE loss in breast cancer patients undergoing immediate breast reconstruction in this study. Wise incision is associated with higher BMI. Total expander capacity predisposed for loss in patients with BMI >23 kg/m2 and a longer drain duration predisposed for loss in patients with BMI <23 kg/m2.
Longer drain duration, particularly in thin patients, larger expander sizes, and use of the Wise pattern incision may drive closer follow-up and hopefully earlier identification of problems. While age is not a modifiable risk factor and weight loss may not be feasible between cancer diagnosis and mastectomy, patients should be made aware that their obesity may put them at risk for more complications and failure of immediate breast reconstruction with expanders. Clinicians should encourage their obese patients to consider this information when comparing relative risks and benefits of autologous versus implant-based reconstruction.
Acknowledgments
This manuscript was presented virtually at Plastic Surgery the Meeting (October 2020). It has not been accepted for publication elsewhere.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://abs.amegroups.com/article/view/10.21037/abs-21-77/rc
Data Sharing Statement: Available at https://abs.amegroups.com/article/view/10.21037/abs-21-77/dss
Peer Review File: Available at https://abs.amegroups.com/article/view/10.21037/abs-21-77/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://abs.amegroups.com/article/view/10.21037/abs-21-77/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional review board of Cooper University Health Care (ID: 18-162) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bertozzi N, Pesce M, Santi P, et al. Tissue expansion for breast reconstruction: Methods and techniques. Ann Med Surg (Lond) 2017;21:34-44. [Crossref] [PubMed]
- Fischer JP, Wes AM, Tuggle CT 3rd, et al. Risk analysis of early implant loss after immediate breast reconstruction: a review of 14,585 patients. J Am Coll Surg 2013;217:983-90. [Crossref] [PubMed]
- Fischer JP, Nelson JA, Au A, et al. Complications and morbidity following breast reconstruction--a review of 16,063 cases from the 2005-2010 NSQIP datasets. J Plast Surg Hand Surg 2014;48:104-14. [Crossref] [PubMed]
- McCarthy CM, Mehrara BJ, Riedel E, et al. Predicting complications following expander/implant breast reconstruction: an outcomes analysis based on preoperative clinical risk. Plast Reconstr Surg 2008;121:1886-92. [Crossref] [PubMed]
- Ilonzo N, Tsang A, Tsantes S, et al. Breast reconstruction after mastectomy: A ten-year analysis of trends and immediate postoperative outcomes. Breast 2017;32:7-12. [Crossref] [PubMed]
- Ota D, Fukuuchi A, Iwahira Y, et al. Identification of complications in mastectomy with immediate reconstruction using tissue expanders and permanent implants for breast cancer patients. Breast Cancer 2016;23:400-6. [Crossref] [PubMed]
- Yan C, Fischer JP, Wes AM, et al. The cost of major complications associated with immediate two-stage expander/implant-based breast reconstruction. J Plast Surg Hand Surg 2015;49:166-71. [Crossref] [PubMed]
- Zahedi S, Colvill K, Lopez M, et al. Implications of Demographics and Socioeconomic Factors in Breast Cancer Reconstruction. Ann Plast Surg 2019;83:388-91. [Crossref] [PubMed]
- Riba LA, Gruner RA, Alapati A, et al. Association between socioeconomic factors and outcomes in breast cancer. Breast J 2019;25:488-92. [Crossref] [PubMed]
- Ghnnam W, Elrahawy A, Moghazy ME. The Effect of Body Mass Index on Outcome of Abdominoplasty Operations. World J Plast Surg 2016;5:244-51. [PubMed]
- Chowdri NA, Qadri SA, Parray FQ, et al. Role of subcutaneous drains in obese patients undergoing elective cholecystectomy: a cohort study. Int J Surg 2007;5:404-7. [Crossref] [PubMed]
- Lim YM, Lew DH, Roh TS, et al. Analysis of factors that affect drainage volume after expander-based breast reconstruction. Arch Plast Surg 2020;47:33-41. [Crossref] [PubMed]
- Murray JD, Elwood ET, Jones GE, et al. Decreasing expander breast infection: A new drain care protocol. Can J Plast Surg 2009;17:17-21. [Crossref] [PubMed]
- Yuen JC, Coleman CA, Erickson SW. Obesity-related Risk Factors in Implant-based Breast Reconstruction Using AlloDerm. Plast Reconstr Surg Glob Open 2017;5:e1231. [Crossref] [PubMed]
- Francis SH, Ruberg RL, Stevenson KB, et al. Independent risk factors for infection in tissue expander breast reconstruction. Plast Reconstr Surg 2009;124:1790-6. [Crossref] [PubMed]
- Khansa I, Hendrick RG Jr, Shore A, et al. Breast reconstruction with tissue expanders: implementation of a standardized best-practices protocol to reduce infection rates. Plast Reconstr Surg 2014;134:11-8. [Crossref] [PubMed]
- Gunn J, Dortch J, TerKonda S, et al. Comparing morbidity rates between wise pattern and standard horizontal elliptical mastectomy incisions in patients undergoing immediate breast reconstruction. Breast J 2019;25:20-5. [Crossref] [PubMed]
- Chen CF, Lin SF, Hung CF, et al. Risk of infection is associated more with drain duration than daily drainage volume in prosthesis-based breast reconstruction: A cohort study. Medicine (Baltimore) 2016;95:e5605. [Crossref] [PubMed]
- Reiffel AJ, Barie PS, Spector JA. A multi-disciplinary review of the potential association between closed-suction drains and surgical site infection. Surg Infect (Larchmt) 2013;14:244-69. [Crossref] [PubMed]
- Chang CW, Tai HC, Cheng NC, et al. Risk factors for complications following immediate tissue expander based breast reconstruction in Taiwanese population. J Formos Med Assoc 2017;116:57-63. [Crossref] [PubMed]
- Wexelman B, Schwartz JA, Lee D, et al. Socioeconomic and geographic differences in immediate reconstruction after mastectomy in the United States. Breast J 2014;20:339-46. [Crossref] [PubMed]
- Cordeiro PG, McCarthy CM. A single surgeon's 12-year experience with tissue expander/implant breast reconstruction: part I. A prospective analysis of early complications. Plast Reconstr Surg 2006;118:825-31. [Crossref] [PubMed]
Cite this article as: Bolshem B, Fahey AL, Melillo AM, Rodby K, Rapaport G, Gaughan JP, Matthews MS. Identification of factors that predict premature tissue expander loss in immediate breast reconstruction. Ann Breast Surg 2023;7:4.