
Immediate or delayed breast reconstruction: the aspects of timing, a narrative review
Introduction
Aside from non-melanoma skin cancers, breast cancer is the most common malignancy affecting women worldwide (1). The last few decades have seen a growth in the number of both immediate and delayed breast reconstruction following mastectomy as breast reconstruction becomes more sought after (2-4). In the United States, the Women’s Health and Cancer Rights Act of 1998 compelled payers to provide benefits for mastectomy-related services, including all reconstruction stages and procedures for symmetry (2). These procedures are also covered in tax-funded healthcare systems.
Bilateral mastectomies have become increasingly common, as a risk reduction procedure, often asked by patients (2). As subsequent breast reconstructions also become more popular, choosing when and how to reconstruct the breasts is exceedingly more nuanced. The present study reviews considerations of the aspects of timing when planning breast reconstruction.
Conservative mastectomy, with preservation of the entire skin envelope or nipple sparing procedure, has gained acceptance in recent years, given evidence of comparable prognosis compared to total mastectomy (5-7). Skin preservation allows for optimized reconstructive outcomes by recreating or enhancing breast volume, lower pole contour, symmetry, and appearance (8). By preserving the breast skin envelope, the skin-sparing mastectomy allows for immediate reconstruction closely matched to the preoperative breast’s size and shape (9). We present the following article in accordance with the Narrative Review reporting checklist (available at https://abs.amegroups.com/article/view/10.21037/abs-21-44/rc).
Reconstruction options
Breast reconstruction options can be either implant-based or autologous. Implant-based breast reconstruction (IBBR) accounts for approximately 80% of breast reconstructions in the United States, most of which are performed immediately following mastectomy (3,4). IBBR can be completed in either one or two stages following mastectomy. The advent of reconstruction with acellular dermal matrix (ADM) allowed the surgeon to create a breast in one stage immediately. An ideal candidate for single-stage, or direct-to-implant (DTI), reconstruction is a patient undergoing skin-sparing, nipple-sparing mastectomy with small to medium breast size, grade 1 or 2 ptosis, and favorable skin quality (10). Two-stage reconstruction is achieved with tissue expanders that are exchanged for implants at a later date. In the setting of immediate reconstruction with questionable perfusion to the mastectomy skin flaps, placement of a tissue expander that is partially filled may protect the skin flaps from tension (11). Surgeons began ADM utilization in 2001 to provide coverage for either implants or tissue expanders in breast reconstruction (12). The original description was a submuscular placement of the implant with lower pole ADM supporting the device and obviating the need for tissue expansion. ADM was used to extend the submuscular plane, support the implant in an anatomic position, and define the inferior and lateral breast folds (10).
Autologous breast reconstruction can be achieved with abdominal tissue- pedicled transverse rectus abdominis myocutaneous (TRAM) flap, or most commonly today with perforator microsurgical tissue transfer (free TRAM flap, muscle-sparing TRAM flap, deep inferior epigastric perforator (DIEP) flap, superficial inferior epigastric artery (SIEA) flap- and with non-abdominal tissue- gluteal flap, transverse upper gracilis flap (TUG), PAP (profunda artery perforator flap) or DUG (diagonal upper gracilis flap) varieties, or lumbar artery perforator flap. Additionally, autologous reconstruction can be achieved with a combined autologous and implant reconstruction used in conjunction with any of the above or flaps based on the thoracodorsal artery (the Latissimus Dorsi musculo-cutanous flap or variants of this) or a perforator from this (the TAP flap). The indications, operative techniques, and patient selection factors relating to these flaps are beyond the present study’s scope and are discussed extensively in the literature (11,13).
Timing considerations and relative contraindications
Historically, less than 25 percent of patients in the U.S. underwent immediate reconstruction (3). The evolution of conservative mastectomy surgical techniques and the introduction of ADM have paved the road for the increased popularity of immediate reconstruction (2,14). In women undergoing mastectomy for early-stage breast cancer, rates of breast reconstruction increased from 11.6% in 1998 to 36.4% in 2011 in the U.S. (15). In Denmark, currently about 20 percent of mastectomized women with invasive breast cancer undergo reconstruction, with a small majority being immediate reconstruction, while most women who undergo mastectomy for in situ cancer are reconstructed immediately (personal message, Hölmich).
Advantages of immediate reconstruction include superior aesthetic outcomes, improved levels of psychosocial wellbeing post-mastectomy at least short-term, shorter surgical time, fewer surgical procedures, lower costs, and faster social reintegration when compared to delayed reconstruction (16-25). Immediate reconstruction demands better skin flaps than a simple mastectomy followed by a delayed reconstruction and may increase the risk of complications (see below). The main advantages of delayed reconstruction are that potential complications do not compromise adjuvant treatment. In addition, if postmastectomy radiation is needed, it does not compromise the reconstruction site, and it gives patients more time to consider reconstructive options. Disadvantages of delayed breast reconstruction also include more scarring and somewhat less favorable cosmetic outcomes, as well as additional surgical procedures and probably higher cost (19,21,23).
A large multicenter U.S. study found that delayed reconstruction (of all kinds) were associated with a substantial reduction in complications compared with immediate reconstructions (the risk of major complications was halved). Women undergoing delayed reconstruction had significantly worse pre-reconstruction quality of life scores than women with immediate reconstruction; however, 2-year post-reconstruction scores were similar in the two groups (22). Another large register-based U.S. study found a significantly higher incidence of surgical site infection after immediate (8.9%) compared with delayed (6.0%) and secondary (3.3%) implant reconstructions (meaning any secondary procedure), with similar results for noninfectious wound complications. In contrast, the incidence of surgical site infection was similar after immediate (9.8%), delayed (13.9%), and secondary (11.6%) autologous reconstructions. The study concludes that the risks for complications should be carefully balanced with the psychosocial and technical benefits of immediate reconstruction. Selected high-risk patients may benefit from consideration of delayed rather than immediate implant reconstruction to decrease breast complications after mastectomy (26).
Both immediate and delayed breast reconstruction has been found to be oncologically safe, although high-quality studies are still lacking. A meta-analysis including 31 studies (mostly retrospective single-center studies) with almost 140,000 patients compared patients undergoing mastectomy +/− immediate breast reconstruction (27). Most included studies had moderate quality, and selection bias was present; women with reconstruction were younger and had less lymph node metastases than those who only underwent mastectomy, but no difference in tumor size. The pooled data showed a higher occurrence of post-operative infection among women undergoing reconstruction (risk ratio 1.51, 95% CI: 1.22–1.87; P=0.0001); however, no significant difference in total survival or disease-free survival.
Complications in cancer surgery have been investigated in a few studies and can negatively influence the oncological outcome. The mechanisms involved are unknown but speculated to involve surgical stress, increased inflammatory response with synthesis of growth factors stimulating cancer cells, lowered immune response, and delay of adjuvant treatment (28). These associations have also been found for bowel, lung, and breast cancer surgery (29-32). Of note, two studies evaluated complications in breast reconstruction (33,34). Both studies found more local and distant recurrences in patients with complications compared with those without complications. This is an emerging field; none of the cited studies are large, and the evidence level at best moderate. However, the results call for caution and proper patient selection, in addition to further research protocols.
Potential delay in adjuvant treatment is a significant concern amongst medical and surgical oncologists. A systematic review of 14 studies, including over 5,000 women, of whom about 2,000 had immediate breast reconstruction, evaluated the timing of the adjuvant treatment and found overall that there was no meaningful delay in adjuvant therapy in the reconstruction group (35).
A multicenter prospective cohort study on about 2,500 consecutive patients undergoing mastectomy +/− breast reconstruction (implant-based or autologous) found significantly more complications associated with breast reconstruction than mastectomy alone. However, no overall difference in time to adjuvant therapy was detected. Those with major complications in both groups had their adjuvant therapy significantly later (36). Care should be taken especially in younger women with triple-negative breast cancer, as timely adjuvant therapy has been found to be especially important in this patient group (37,38).
The above allows for the conclusion that immediate breast reconstruction is oncologically safe if adequate precautions are taken; however, care must be taken to avoid complications, and thorough patient selection is therefore critical. If women with risk factors undergo immediate reconstruction, more complications will occur and delay in adjuvant therapy can be expected. Neoadjuvant treatment preoperatively should always be considered.
Despite the numerous benefits, patient selection is therefore critical in evaluating the timing of reconstruction as not all patients are suitable candidates for immediate reconstruction. Delayed reconstruction should be considered for patients with pressing medical comorbidities, obesity, smoking, inflammatory breast cancer, patients going to have post-mastectomy radiation therapy, and for patients distressed regarding their breast cancer diagnosis who are not ready to make treatment decisions (22,39,40).
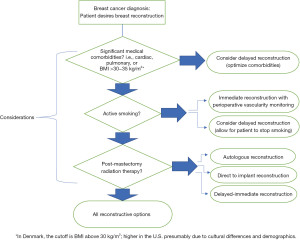
Several absolute and relative contraindications should be considered and discussed in-depth, with the patient and at multidisciplinary tumor board conferences. There is a general consensus that only a few absolute oncologic contraindications for immediate breast reconstruction exist: locally advanced breast cancer and inflammatory breast cancer (9,22). Active infection in the breast area is a surgical contraindication. However, many conditions may present relative contraindications to immediate reconstruction and will be discussed below: increased age, smoking, obesity, comorbidities, risk of delaying adjuvant therapy. Figure 1 depicts the authors algorithm for deciding for immediate or delayed breast reconstruction. Some cultural and national differences exist among the authors’ practice which is included in the algorithm.
Age
There has previously been debate about whether increased age is a contraindication to immediate reconstruction. Studies have found increasing age to be associated with infection and skin necrosis, presumably due to decreased vascularity and comorbidity (41-44). Studies have also shown that immediate breast reconstruction is safe in elderly patients if pre-existing medical conditions are optimized pre-operatively, and thus, a patient’s age alone is not a contraindication to immediate reconstruction (45-47).
Smoking
Delaying reconstruction is preferred in patients who are actively smoking, which will give the patient time to stop. Several studies have found an approximately doubled risk of complications in smokers undergoing breast reconstruction (41-44,48,49). There are also studies indicating that earlier smoking is associated with a higher risk of skin necrosis (48). If reconstruction is performed in an active smoker, peri-operative monitoring of the vascularity of the skin flaps is therefore advisable (50). A large meta-analysis found current smoking and former smoking of 20 pack-years or more to be associated with a significantly increased risk of recurrence and death, both disease-specific and overall (51). Active smoking is therefore considered an important relative contraindication for immediate reconstruction. In Denmark, this also applies to delayed reconstruction. The authors would only consider immediate reconstruction in light smokers without any other risk factors for complications.
BMI
The risk of complications such as infection, skin necrosis and loss of implant is increased in overweight patients and about double the risk of normal weight (41,44,52,53). Overweight patients often have large and broad-based breasts, which will yield a large wound area during the skin-sparing mastectomy. Larger flaps or implants are generally needed; all of these factors are probably adding to the increased risk of complications. In many national guidelines, BMI above 30 kg/m2 is considered at least a relative contraindication (44,54). Different countries and cultures have different proportions of obese patients and guidelines often reflects this (55,56). Among the authors, discrepancy exists as BMI 30 is used as cut off in Denmark (and generally so in the Nordic countries), while the upper limit in the US is higher.
PMRT
In patients requiring PMRT, the optimal timing and method of breast reconstruction are controversial (57). Generally, plastic surgeons and surgical oncologists advise completion of radiation therapy prior to reconstructing the breast to avoid higher rates of complications of the reconstructed breast receiving PMRT (57-59). The traditional approach calls for tissue expander exchange for the permanent breast implant after the conclusion of PMRT however the authors prefer exchange to implant prior to the radiation, if possible, in order to allow surgery in a non-radiated field. If not possible, the use of a counter incision at the IMF or outside the field is preferred to one over the central portion of the breast. One study found that nearly 50% of implant-based breast reconstruction patients who underwent radiation may require revisions to their reconstruction (60). A meta-analysis evaluating complications including in pre-mastectomy versus postmastectomy radiation therapy generally in two-staged implant reconstruction and found similar and high complication rates and failures (17% versus 20%) (61). The commonly accepted view is that reconstruction with autologous tissue is superior to implant reconstruction within an irradiated operative field. However, autologous tissue reconstructions can also be negatively affected by PMRT (49,57,58). In contrast, a prospective study demonstrated immediate autologous reconstruction in the setting of PMRT to be a safe option that did not negatively affect breast aesthetics nor the patient’s quality of life (62). They attribute their findings to advances in radiation techniques such as three-dimensional planning and simple intensity modulation, which allow for greater dose homogeneity within the treatment field (62). There is an abundance of evidence supporting the oncological safety of immediate reconstruction (27). However, the risk a reconstructed breast may pose on comprimising radiation delivery is still a subject of debate (63). The authors generally prefer a delayed autologous reconstruction in case of radiation therapy, but if the patient is not willing to this, an immediate direct-to-implant reconstruction is preferable. We would try to avoid radiation towards an expander, if possible; since it may more difficult to plan the radiation field in a patient with an expander than with a permanent implant, meaning a potentially higher risk of additional radiation to the lungs and the heart or an insufficient dosage distribution (63). In addition, to overcome expansion during chemotherapy which is often given before radiation therapy and performing exchange before radiation therapy can be demanding.
Chemotherapy
As discussed previously, post-reconstruction chemotherapy has not been found to be generally compromised by the reconstruction (35,36). Regarding neoadjuvant chemotherapy in the setting of immediate reconstruction, a recent meta-analysis concluded that immediate reconstruction following neoadjuvant chemotherapy is safe with acceptable post-operative complication levels. The meta-analysis found that neoadjuvant therapy may result in slightly increased implant loss levels; however, there was no delay in commencement of adjuvant therapy (64).
Conclusions
Patient preference, risk factors and oncologic considerations are always important when planning reconstruction timing. Immediate reconstruction offers many advantages over delayed reconstruction, however, long-term patient-reported outcomes have been found similar, which we should not forget. The authors prefer immediate reconstruction when feasible. The timing and technique of reconstruction should be decided on a case-by-case basis after a thorough discussion with the patient and preferably also in multidisciplinary meetings.
This controversial topic is one that is debated over and over again. Consensus among the surgeons, chemotherapists, and radiation oncologists is the ideal and meetings which encourage this type of dialogue should be routine.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Tine Engberg Damsgaard and Jørn Bo Thomsen) for the series “Breast Reconstruction—The True Multidisciplinary Approach” published in Annals of Breast Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://abs.amegroups.com/article/view/10.21037/abs-21-44/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://abs.amegroups.com/article/view/10.21037/abs-21-44/coif). The series “Breast Reconstruction—The True Multidisciplinary Approach” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359-86. [Crossref] [PubMed]
- Panchal H, Matros E. Current Trends in Postmastectomy Breast Reconstruction. Plast Reconstr Surg 2017;140:7S-13S. [Crossref] [PubMed]
- Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg 2013;131:15-23. [Crossref] [PubMed]
- Cemal Y, Albornoz CR, Disa JJ, et al. A paradigm shift in U.S. breast reconstruction: Part 2. The influence of changing mastectomy patterns on reconstructive rate and method. Plast Reconstr Surg 2013;131:320e-6e. [Crossref] [PubMed]
- Spear SL, Willey SC, Feldman ED, et al. Nipple-sparing mastectomy for prophylactic and therapeutic indications. Plast Reconstr Surg 2011;128:1005-14. [Crossref] [PubMed]
- Endara M, Chen D, Verma K, et al. Breast reconstruction following nipple-sparing mastectomy: a systematic review of the literature with pooled analysis. Plast Reconstr Surg 2013;132:1043-54. [Crossref] [PubMed]
- Meshulam-Derazon S, Shay T, Lewis S, et al. Immediate Breast Reconstruction: Comparative Outcome Study of One-Stage Direct-to-Implant and Two-Stage/Tissue Expander Techniques. Isr Med Assoc J 2018;20:340-4. [PubMed]
- Nahabedian MY. Implant-based breast reconstruction following conservative mastectomy: one-stage vs. two-stage approach. Gland Surg 2016;5:47-54. [PubMed]
- Cho BC, McCready DR. Oncologic principles in breast reconstruction. Clin Plast Surg 2007;34:1-13; abstract v. [Crossref] [PubMed]
- Salzberg CA. Direct-to-implant breast reconstruction. Clin Plast Surg 2012;39:119-26. [Crossref] [PubMed]
- Zhong T, McCarthy CM, Price AN, et al. Evidence-based medicine: breast reconstruction. Plast Reconstr Surg 2013;132:1658-69. [Crossref] [PubMed]
- Salzberg CA. Nonexpansive immediate breast reconstruction using human acellular tissue matrix graft (AlloDerm). Ann Plast Surg 2006;57:1-5. [Crossref] [PubMed]
- Macadam SA, Bovill ES, Buchel EW, et al. Evidence-Based Medicine: Autologous Breast Reconstruction. Plast Reconstr Surg 2017;139:204e-29e. [Crossref] [PubMed]
- Zenn MR, Salzberg CA. A Direct Comparison of Alloderm-Ready to Use (RTU) and DermACELL in Immediate Breast Implant Reconstruction. Eplasty 2016;16:e23. [PubMed]
- Kummerow KL, Du L, Penson DF, et al. Nationwide trends in mastectomy for early-stage breast cancer. JAMA Surg 2015;150:9-16. [Crossref] [PubMed]
- Al-Ghazal SK, Sully L, Fallowfield L, et al. The psychological impact of immediate rather than delayed breast reconstruction. Eur J Surg Oncol 2000;26:17-9. [Crossref] [PubMed]
- D'Souza N, Darmanin G, Fedorowicz Z. Immediate versus delayed reconstruction following surgery for breast cancer. Cochrane Database Syst Rev 2011;CD008674. [Crossref] [PubMed]
- Howes BH, Watson DI, Xu C, et al. Quality of life following total mastectomy with and without reconstruction versus breast-conserving surgery for breast cancer: A case-controlled cohort study. J Plast Reconstr Aesthet Surg 2016;69:1184-91. [Crossref] [PubMed]
- Kroll SS, Coffey JA Jr, Winn RJ, et al. A comparison of factors affecting aesthetic outcomes of TRAM flap breast reconstructions. Plast Reconstr Surg 1995;96:860-4. [Crossref] [PubMed]
- Ng SK, Hare RM, Kuang RJ, et al. Breast Reconstruction Post Mastectomy: Patient Satisfaction and Decision Making. Ann Plast Surg 2016;76:640-4. [Crossref] [PubMed]
- Elkowitz A, Colen S, Slavin S, et al. Various methods of breast reconstruction after mastectomy: an economic comparison. Plast Reconstr Surg 1993;92:77-83. [Crossref] [PubMed]
- Yoon AP, Qi J, Brown DL, et al. Outcomes of immediate versus delayed breast reconstruction: Results of a multicenter prospective study. Breast 2018;37:72-9. [Crossref] [PubMed]
- Khoo A, Kroll SS, Reece GP, et al. A comparison of resource costs of immediate and delayed breast reconstruction. Plast Reconstr Surg 1998;101:964-8; discussion 969-70. [Crossref] [PubMed]
- Prantl L, Moellhoff N, von Fritschen U, et al. Immediate versus secondary DIEP flap breast reconstruction: a multicenter outcome study. Arch Gynecol Obstet 2020;302:1451-9. [Crossref] [PubMed]
- Filip CI, Jecan CR, Raducu L, et al. Immediate Versus Delayed Breast Reconstruction for Postmastectomy Patients. Controversies and Solutions. Chirurgia (Bucur) 2017;112:378-86. [Crossref] [PubMed]
- Olsen MA, Nickel KB, Fox IK, et al. Comparison of Wound Complications After Immediate, Delayed, and Secondary Breast Reconstruction Procedures. JAMA Surg 2017;152:e172338. [Crossref] [PubMed]
- Zhang P, Li CZ, Wu CT, et al. Comparison of immediate breast reconstruction after mastectomy and mastectomy alone for breast cancer: A meta-analysis. Eur J Surg Oncol 2017;43:285-93. [Crossref] [PubMed]
- Beecher SM. The Impact of Surgical Complications on Cancer Recurrence Rates: A Literature Review. Oncol Res Treat 2018;41:478-82. [Crossref] [PubMed]
- Mirnezami A, Mirnezami R, Chandrakumaran K, et al. Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg 2011;253:890-9. [Crossref] [PubMed]
- Krarup PM, Nordholm-Carstensen A, Jorgensen LN, et al. Anastomotic leak increases distant recurrence and long-term mortality after curative resection for colonic cancer: a nationwide cohort study. Ann Surg 2014;259:930-8. [Crossref] [PubMed]
- Nojiri T, Hamasaki T, Inoue M, et al. Long-Term Impact of Postoperative Complications on Cancer Recurrence Following Lung Cancer Surgery. Ann Surg Oncol 2017;24:1135-42. [Crossref] [PubMed]
- Murthy BL, Thomson CS, Dodwell D, et al. Postoperative wound complications and systemic recurrence in breast cancer. Br J Cancer 2007;97:1211-7. [Crossref] [PubMed]
- Beecher SM, O'Leary DP, McLaughlin R, et al. Influence of complications following immediate breast reconstruction on breast cancer recurrence rates. Br J Surg 2016;103:391-8. [Crossref] [PubMed]
- Lee KT, Jung JH, Mun GH, et al. Influence of complications following total mastectomy and immediate reconstruction on breast cancer recurrence. Br J Surg 2020;107:1154-62. [Crossref] [PubMed]
- Xavier Harmeling J, Kouwenberg CA, Bijlard E, et al. The effect of immediate breast reconstruction on the timing of adjuvant chemotherapy: a systematic review. Breast Cancer Res Treat 2015;153:241-51. [Crossref] [PubMed]
- O'Connell RL, Rattay T, Dave RV, et al. The impact of immediate breast reconstruction on the time to delivery of adjuvant therapy: the iBRA-2 study. Br J Cancer 2019;120:883-95. [Crossref] [PubMed]
- Colleoni M, Bonetti M, Coates AS, et al. Early start of adjuvant chemotherapy may improve treatment outcome for premenopausal breast cancer patients with tumors not expressing estrogen receptors. The International Breast Cancer Study Group. J Clin Oncol 2000;18:584-90. [Crossref] [PubMed]
- de Melo Gagliato D, Lei X, Giordano SH, et al. Impact of Delayed Neoadjuvant Systemic Chemotherapy on Overall Survival Among Patients with Breast Cancer. Oncologist 2020;25:749-57. [Crossref] [PubMed]
- Ananthakrishnan P, Lucas A. Options and considerations in the timing of breast reconstruction after mastectomy. Cleve Clin J Med 2008;75:S30-3. [Crossref] [PubMed]
- Ho AY, Hu ZI, Mehrara BJ, et al. Radiotherapy in the setting of breast reconstruction: types, techniques, and timing. Lancet Oncol 2017;18:e742-53. [Crossref] [PubMed]
- McCarthy CM, Mehrara BJ, Riedel E, et al. Predicting complications following expander/implant breast reconstruction: an outcomes analysis based on preoperative clinical risk. Plast Reconstr Surg 2008;121:1886-92. [Crossref] [PubMed]
- Mlodinow AS, Fine NA, Khavanin N, et al. Risk factors for mastectomy flap necrosis following immediate tissue expander breast reconstruction. J Plast Surg Hand Surg 2014;48:322-6. [Crossref] [PubMed]
- Tang R, Coopey SB, Colwell AS, et al. Nipple-Sparing Mastectomy in Irradiated Breasts: Selecting Patients to Minimize Complications. Ann Surg Oncol 2015;22:3331-7. [Crossref] [PubMed]
- Mureau MAMBreast Reconstruction Guideline Working Group. Dutch breast reconstruction guideline. J Plast Reconstr Aesthet Surg 2018;71:290-304. [Crossref] [PubMed]
- Preminger BA, Trencheva K, Chang CS, et al. Improving access to care: breast surgeons, the gatekeepers to breast reconstruction. J Am Coll Surg 2012;214:270-6. [Crossref] [PubMed]
- Howard-McNatt M, Forsberg C, Levine EA, et al. Breast cancer reconstruction in the elderly. Am Surg 2011;77:1640-3. [Crossref] [PubMed]
- Veronesi P, Ballardini B, De Lorenzi F, et al. Immediate breast reconstruction after mastectomy. Breast 2011;20:S104-7. [Crossref] [PubMed]
- Goodwin SJ, McCarthy CM, Pusic AL, et al. Complications in smokers after postmastectomy tissue expander/implant breast reconstruction. Ann Plast Surg 2005;55:16-19; discussion 19-20. [Crossref] [PubMed]
- Rogers NE, Allen RJ. Radiation effects on breast reconstruction with the deep inferior epigastric perforator flap. Plast Reconstr Surg 2002;109:1919-24; discussion 1925-6. [Crossref] [PubMed]
- Lauritzen E, Damsgaard TE. Use of Indocyanine Green Angiography decreases the risk of complications in autologous- and implant-based breast reconstruction: A systematic review and meta-analysis. J Plast Reconstr Aesthet Surg 2021;74:1703-17. [Crossref] [PubMed]
- Pierce JP, Patterson RE, Senger CM, et al. Lifetime cigarette smoking and breast cancer prognosis in the After Breast Cancer Pooling Project. J Natl Cancer Inst 2014;106:djt359. [Crossref] [PubMed]
- Woerdeman LA, Hage JJ, Hofland MM, et al. A prospective assessment of surgical risk factors in 400 cases of skin-sparing mastectomy and immediate breast reconstruction with implants to establish selection criteria. Plast Reconstr Surg 2007;119:455-63. [Crossref] [PubMed]
- Heidekrueger PI, Fritschen U, Moellhoff N, et al. Impact of body mass index on free DIEP flap breast reconstruction: A multicenter cohort study. J Plast Reconstr Aesthet Surg 2021;74:1718-24. [Crossref] [PubMed]
- American Society of Plastic Surgeons. Evidence-Based Clinical Practice Guideline: Breast Reconstruction with Expanders and Implants. Published online 2013. Accessed August 28, 2021. Available online: https://www.plasticsurgery.org/Documents/Health-Policy/Guidelines/guideline-2013-breast-recon-expanders-implants.pdf
- Queeensland Health, Department of Health. Breast Reconstruction Surgery. Published online January 17, 2019. Accessed August 28, 2021. Available online: https://www.health.qld.gov.au/__data/assets/pdf_file/0029/813719/qh-imp-463.pdf
- Breast Reconstruction Following Prophylactic or Therapeutic Mastectomy for Breast Cancer, Alberta Health Services. Accessed August 28, 2021. Available online: https://www.albertahealthservices.ca/assets/info/hp/cancer/if-hp-cancer-guide-br016-breast-reconstruction.pdf
- Kronowitz SJ, Robb GL. Breast reconstruction with postmastectomy radiation therapy: current issues. Plast Reconstr Surg 2004;114:950-60. [Crossref] [PubMed]
- Tran NV, Chang DW, Gupta A, et al. Comparison of immediate and delayed free TRAM flap breast reconstruction in patients receiving postmastectomy radiation therapy. Plast Reconstr Surg 2001;108:78-82. [Crossref] [PubMed]
- Lee M, Reinertsen E, McClure E, et al. Surgeon motivations behind the timing of breast reconstruction in patients requiring postmastectomy radiation therapy. J Plast Reconstr Aesthet Surg 2015;68:1536-42. [Crossref] [PubMed]
- Spear SL, Onyewu C. Staged breast reconstruction with saline-filled implants in the irradiated breast: recent trends and therapeutic implications. Plast Reconstr Surg 2000;105:930-42. [Crossref] [PubMed]
- Momoh AO, Ahmed R, Kelley BP, et al. A systematic review of complications of implant-based breast reconstruction with prereconstruction and postreconstruction radiotherapy. Ann Surg Oncol 2014;21:118-24. [Crossref] [PubMed]
- Billig J, Jagsi R, Qi J, et al. Should Immediate Autologous Breast Reconstruction Be Considered in Women Who Require Postmastectomy Radiation Therapy? A Prospective Analysis of Outcomes. Plast Reconstr Surg 2017;139:1279-88. [Crossref] [PubMed]
- Motwani SB, Strom EA, Schechter NR, et al. The impact of immediate breast reconstruction on the technical delivery of postmastectomy radiotherapy. Int J Radiat Oncol Biol Phys 2006;66:76-82. [Crossref] [PubMed]
- Varghese J, Gohari SS, Rizki H, et al. A systematic review and meta-analysis on the effect of neoadjuvant chemotherapy on complications following immediate breast reconstruction. Breast 2021;55:55-62. [Crossref] [PubMed]
Cite this article as: Hölmich LR, Sayegh F, Salzberg CA. Immediate or delayed breast reconstruction: the aspects of timing, a narrative review. Ann Breast Surg 2023;7:6.

