
A novel surgical approach to treat lymphangioma of the breast and prevent seroma—a case report
Highlight box
Key findings
• Quilting using a barbed suture to secure the skin flap to the underlying breast tissue or muscle was an effective technique to prevent seroma formation in this case of large breast lymphangioma.
• The patient reported satisfaction with the cosmetic outcome.
What is known and what is new?
• Quilting reduces the rate of seroma formation after mastectomy.
• A recent study shows that rows of Stratafix sutures are the most effective quilting technique.
• This is the first case in the literature describing the quilting technique to reduce seroma formation and achieve acceptable cosmesis in a large lymphangioma of the breast, with positive patient reported outcomes.
• The use of Stratafix for quilting in this setting is novel and contributed to the patient’s rapid recovery.
What is the implication, and what should change now?
• Surgical excision is definitive treatment of breast lymphangioma.
• Quilting is the optimal technique to prevent seroma formation.
• Surgical excision with Stratafix quilting should be adopted to treat symptomatic breast lymphangioma.
Introduction
Lymphangiomas are benign lymphatic tumours which are histologically composed of networks of endothelium-lined spaces (1). They can be classified as simple (capillary) or cavernous lymphangioma (cystic hygroma). On histological assessment, simple lymphangiomas can be distinguished from capillaries only by the absence of blood cells (1). Cavernous lymphangiomas are typically found in the neck and axilla of children (2). These lesions are composed of dilated endothelial lined lymphatic spaces separated by connective tissue stroma with lymphoid aggregates (1).
Lymphangioma of the breast is extremely rare, with few cases described in the literature. Table 1 summarises previously published cases of breast lymphangioma. In previously published case reports, surgical excision has been a successful treatment modality (3-8). There is no evidence of successful management with aspiration or steroid injection. Quilting in breast surgery typically refers to the use of sutures to secure the skin flaps to the underlying pectoralis major muscle. This technique significantly reduced seroma formation in mastectomy patients (9,10). There is a paucity of evidence within the literature describing surgical techniques, in cases of lymphangioma, to reduce seroma formation and achieve acceptable cosmesis. There are no comments on patient satisfaction with cosmesis in published case reports.
Table 1
| Authors | Age, years | Intervention | Outcome | Follow-up |
|---|---|---|---|---|
| Ogun et al. (3) | 38 | Surgical excision | No complications or recurrence | 5 years |
| Park et al. (4) | 37 | Surgical excision | No complications or recurrence | 6 months |
| Torcasio et al. (5) | 26 | Surgical excision | No complications or recurrence | 2 years |
| Agarwal et al. (6) | 36 | Surgical excision | No complications or recurrence | Not stated |
| Rusdianto et al. (7) | 20 | Surgical excision | No complications or recurrence | 3 weeks |
| Principe et al. (8) | 27 | Surgical excision | No complications or recurrence | Immediate post-operative only |
This case describes a novel surgical approach to treatment of lymphangioma of the breast, focusing on the application of quilting which reduces the dead space within the cavity after surgical excision to eliminate the risk of seroma formation and maintain acceptable cosmesis. The operative approach has not previously been described. We present this article in accordance with the CARE reporting checklist (available at https://abs.amegroups.com/article/view/10.21037/abs-24-13/rc).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institution of NHS Lothian Caldicott Office, as approved by the local Caldicott Guardian (Caldicott Application No. 2315) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
This 44-year-old lady presented with a left sided breast lump in the upper outer quadrant. She described recurrence of the lump following multiple aspirations of fluid over an 18-month period (within a different health board), the last occasion being 4 months previously. She had no significant past medical history. She had no systemic symptoms and no previous history of breast or axillary disease. There was no family history of breast or ovarian cancer.
On clinical examination there was a 10 cm mass lesion in the upper outer quadrant of the left breast. There were multiple palpable lymph nodes in both axillae and a recent history of coronavirus disease 2019 (COVID-19) vaccination.
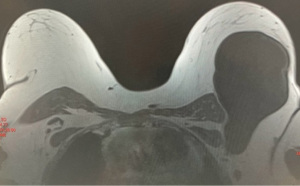
Magnetic resonance imaging (MRI) scan revealed a 16 cm × 8 cm × 8 cm fluid collection in the left upper outer quadrant extending into the axilla to lie under pectoralis major muscle (Figure 1). Breast ultrasound scan revealed a large cystic lesion measuring 79 mm. Aspiration of 375 mL of straw colour fluid was carried out in the clinic setting using a large bore (14 Gauge) cannula with ultrasound guidance and cytology showed abundant lymphocytes and no atypical cells. Ultrasound scan of the axilla revealed multiple enlarged nodes. On a repeat ultrasound scan of the left axilla, the nodes remained enlarged, and a core biopsy showed features in keeping with a reactive lymph node. This patient initially underwent aspiration every second month, using the previously mentioned technique, with the synthetic glucocorticoid Triamcinolone being injected on two occasions. The patients primary concern was discomfort and a large unsightly mass. Repeated aspirations, with re-accumulation of the fluid, brought temporary symptomatic relief but did not provide long-term resolution.
Following 8 aspiration procedures over a period of 14 months, with no decrease in size, a decision was taken to excise the lesion. Following an axillary skin crease incision, the lesion was excised intact by a combination of sharp and blunt dissection, care was required in the upper axilla where the cystic lesion was closely applied to a duplicate axillary vein. Attached to the lesion were several axillary nodes that were pigmented from nearby tattoos. Following complete excision, the large residual cavity was closed in multiple layers using a running suture technique with a barbed 2/0 Stratafix suture (Figure 2). The wound was closed with 3/0 Stratafix and Monocryl.

The specimen weighed 173 grams and measured 150 mm × 100 mm × 25 mm (Figure 3). On microscopy there were 2 main components. The first was varied size interweaved vascular channels, in some places large and cystically dilated, occasionally showing a papillary/villo-nodular appearance reminiscent of reactive synovium (Figure 3). They were lined by flat endothelium, lacking atypia. The channels were associated with reactive lymphoid tissue, with large germinal centres, some of which contained black pigment (thought to be tattoo pigment) and background fibrosis (Figure 3B). Their reactive nature was well supported by their normal immunohistochemical profile for selected markers. The features were consistent with a large benign lymphangioma with secondary inflammation and reactive nodal change.

On review 4 weeks post-operatively, there was no seroma formation or recurrence of lymphangioma. The patient was pleased with the cosmetic outcome and the discomfort associated with the lesion had disappeared (Figure 4). On review fifteen months following surgery, there has been no seroma formation, cosmesis is excellent and there is no indication for lipofilling.

Discussion
Lymphangioma of the breast is a rare entity and surgical excision is the mainstay of treatment. There is no evidence to support a conservative approach in the current literature.
Seroma formation is common following axillary and breast surgery due to the potential space that is left behind which accumulates fluid. Seromas can be complicated by infection, discomfort, can have a negative impact on patients due to multiple visits to hospital and can cause breast distortion as the seroma cavity contracts. Although more commonly described following breast surgery for malignancy, there is a need to effectively prevent seroma formation following excision of large breast lymphangiomas. Different methods described to reduce seroma formation include local steroid injection, fibrin glue, drain insertion and quilting.
Triamcinolone is a synthetic glucocorticoid which has been shown to effectively reduce donor site seroma formation after autologous latissimus dorsi reconstruction (11). In a double-blind randomised controlled trial of 52 patients, intra-cavity triamcinolone injection, following seroma aspiration, reduced the need for further aspiration, total number of aspirations, total volume aspirated and total time to dryness. Local triamcinolone has also been shown to significantly reduce seroma accumulation, and supressed levels of inflammatory markers, in a randomised controlled trial of abdominoplasty patients (12). In a randomised clinical trial of 212 women having mastectomy and sentinel lymph node biopsy, methylprednisolone into the wound cavity on the first day significantly prevented seroma formation (46% in methylprednisolone group, 67% in control group, P<0.001) with no complications (13). These patient cohorts are clearly very different from a patient with lymphangioma, with some patients receiving adjuvant chemotherapy and radiotherapy. The evidence from the patient treated here is that triamcinolone is not effective in the treatment of lymphoceles.
In a meta-analysis of 11 randomised controlled trials including 2,009 mastectomy patients, quilting significantly reduced seroma formation compared with conventional closure (P<0.001, RR: 0.367) (9). These findings were supported when a further meta-analysis of 21 studies including 3,473 patients was published in 2022, showing reduced rates of seroma, total volume of drainage, days to drain removal and length of stay in patients following mastectomy +/− axillary lymph node dissection (10). Compared to fibrin glue or triamcinolone, quilting emerged as the optimal strategy to decrease donor-site seroma following latissimus dorsi flap reconstruction (quilting group 5%, control 34.5%; fibrin, 27.6%; and triamcinolone 37.6%) in a randomised trial of 96 breast cancer patients (14). There was no difference in complications. A recent study shows that rows of Stratafix sutures as used in this patient are the most effective quilting technique (15). This is the first case to describe the use of quilting to prevent seroma formation in a case of large breast lymphocele.
An alternative to surgical excision, presented in the literature in the form of a case report, is the combination of lymphaticovenular anastomosis (LVA), and ethanol sclerotherapy which closes the dead space (16). LVA enables lymphatic fluid to flow directly from lymphatic channels to the vascular system, stopping the flow of lymphatic fluid within the cyst and maintain effective drainage. The authors describe resolution of a large cystic lymphangioma, arising from the axilla to the sub-clavicular area between the pectoral muscles, with no subsequent lymphoedema or recurrence at 18 months (16). Key benefits of this approach are the minimally invasive nature of the surgery. However, the lymphatics must be detectable, and this is not always the case if the lymphocele is large, persistent or infected. LVA is a delicate microsurgical procedure that requires subspecialist training and specialised instruments. Open surgical excision offers definitive treatment for lymphangioma in cases not amenable to LVA, and is feasible within healthcare systems where specialist microsurgery such as LVA is not routinely available.
Aesthetic outcome is a factor that must not be overlooked in surgery for benign and malignant breast disease. In a study of patients who had breast surgery and radiotherapy, poor patient reported cosmetic satisfaction was independently associated with impaired quality of life, body image, and lower emotional and social functioning (17). Seromas can adversely affect cosmesis after breast surgery. The so-called ‘ideal’ female breast is complex and is influenced by culture, race and body type. It is critical to explore each individual patients’ preferences and make shared decisions to arrive at the optimal outcome, in terms of the management of breast disease and achieving an acceptable cosmetic outcome. Reducing seroma formation by quilting in our experience improves cosmetic outcomes.
The surgical approach in this case was successful and strengths included complete excision of the large lesion through a cosmetically acceptable skin incision and the application of the quilting technique to prevent seroma formation within a large potential space. Pre-operative MRI scanning was important to delineate the anatomy of the tumour in relation to major axillary vessels. The cosmetic result was very good from the perspective of both the patient and the surgeon.
The delay between first presentation and surgery was due to a variety of factors. These include initial diagnostic uncertainty, patient factors including re-locating to a new health board, inexperience in treating this rare entity and the timing during the COVID-19 pandemic when non-urgent operations were not taking place locally. Once seen by a senior surgeon the operation was planned and executed in a timely manner with an excellent outcome. A key limitation of this article is that this is a single case report. However, the same approach has been adopted in many different scenarios. This includes removing implants with their capsules and closing the space by quilting and its use in two patients with augmentation with polyacrylamide hydrogel where we drained the gel and excised the pseudocapsule. Thus the technique of quilting as described here can be applied to any situation where, following breast surgery, there are large spaces in the breast that need to be closed. This case report thus adds to the current literature by describing a novel approach in such patients of using quilting with Stratafix to prevent seroma.
Conclusions
In this case report, surgical excision was the definitive treatment of breast lymphangioma. Quilting using a barbed suture to secure the skin flap to the underlying breast tissue or muscle was a successful technique with no seroma formation. The use of Stratafix for quilting in this setting is novel and contributed to the patients rapid recovery.
Acknowledgments
The authors would like to thank Dr Stuart Thomas for providing valuable insights into the pathological reporting of this case.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://abs.amegroups.com/article/view/10.21037/abs-24-13/rc
Peer Review File: Available at https://abs.amegroups.com/article/view/10.21037/abs-24-13/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://abs.amegroups.com/article/view/10.21037/abs-24-13/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the NHS Lothian Caldicott Office, as approved by the local Caldicott Guardian (Caldicott Application No. 2315) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kumar V, Abbas AK, Aster JC. Robbins Basic Pathology. Ninth Edition. Elsevier; 2012.
- Grasso DL, Pelizzo G, Zocconi E, et al. Lymphangiomas of the head and neck in children. Acta Otorhinolaryngol Ital 2008;28:17-20. [PubMed]
- Ogun GO, Oyetunde O, Akang EE. Cavernous lymphangioma of the breast. World J Surg Oncol 2007;5:69. [Crossref] [PubMed]
- Park T, Lee HS, Jung EJ, et al. Concomitant breast and axillary lymphangioma in an adult: A case report and a review of the literature. Medicine (Baltimore) 2018;97:e12946. [Crossref] [PubMed]
- Torcasio A, Veneroso S, Amabile MI, et al. Cystic hygroma of the breast: a rare lesion. Tumori 2006;92:347-50. [Crossref] [PubMed]
- Agarwal S, Doctor M, Ruidas S, et al. Cystic lymphangioma of breast: a rare presentation. BMJ Case Rep 2020;13:e235040. [Crossref] [PubMed]
- Rusdianto E, Murray M, Davis J, et al. Adult cystic lymphangioma in the inner quadrant of the breast-Rare location for a rare disease: A case report. Int J Surg Case Rep 2016;20:123-6. [Crossref] [PubMed]
- Principe DR, Rubin J, Raicu A, et al. Massive adult cystic lymphangioma of the breast. J Surg Case Rep 2019;2019:rjz027. [Crossref] [PubMed]
- Eliav T, Novack V, Krieger Y. Effect of quilting on seroma formation in mastectomies: A meta-analysis. Surg Oncol 2021;39:101665. [Crossref] [PubMed]
- Morarasu S, Clancy C, Ghetu N, et al. Impact of Quilting Sutures on Surgical Outcomes After Mastectomy: A Systematic Review and Meta-Analysis. Ann Surg Oncol 2022;29:3785-97. [Crossref] [PubMed]
- Taghizadeh R, Shoaib T, Hart AM, et al. Triamcinolone reduces seroma re-accumulation in the extended latissimus dorsi donor site. J Plast Reconstr Aesthet Surg 2008;61:636-42. [Crossref] [PubMed]
- Anker AM, Felthaus O, Prantl L, et al. Local Triamcinolone Treatment Affects Inflammatory Response in Seroma Exudate of Abdominoplasty Patients: A Randomized Controlled Trial. Plast Reconstr Surg 2021;147:345-54. [Crossref] [PubMed]
- Qvamme G, Axelsson CK, Lanng C, et al. Randomized clinical trial of prevention of seroma formation after mastectomy by local methylprednisolone injection. Br J Surg 2015;102:1195-203. [Crossref] [PubMed]
- Hart AM, Duggal C, Pinell-White X, et al. A Prospective Randomized Trial of the Efficacy of Fibrin Glue, Triamcinolone Acetonide, and Quilting Sutures in Seroma Prevention after Latissimus Dorsi Breast Reconstruction. Plast Reconstr Surg 2017;139:854e-63e. [Crossref] [PubMed]
- van Zeelst LJ, van der Waal DC, Keemers-Gels ME, et al. Effect of different quilting techniques on seroma formation after breast surgery: retrospective study. BJS Open 2023;7:zrac171. [Crossref] [PubMed]
- Yoshida S, Imai H, Roh S, et al. Combined Treatment with Lymphaticovenular Anastomosis and Ethanol Sclerotherapy for Cystic Lymphangioma in a Limb. Plast Reconstr Surg Glob Open 2022;10:e4348. [Crossref] [PubMed]
- Batenburg MCT, Gregorowitsch ML, Maarse W, et al. Patient-reported cosmetic satisfaction and the long-term association with quality of life in irradiated breast cancer patients. Breast Cancer Res Treat 2020;179:479-89. [Crossref] [PubMed]
Cite this article as: Swan R, Revie E, Dixon M. A novel surgical approach to treat lymphangioma of the breast and prevent seroma—a case report. Ann Breast Surg 2025;9:8.

