
Polymorphous adenocarcinoma of the breast: a case report and review of the literature
Highlight box
Key findings
• A 56-year-old female who presented with smooth, mobile, superficial breast nodule was diagnosed with polymorphous adenocarcinoma (PAC) of the breast.
What is known and what is new?
• PAC of the breast is a rare tumor that is morphologically similar to salivary gland tumors.
• This is the fifth reported case of PAC of the breast which is unique from previous reports in the way it presented as benign-appearing dermal nodule.
What is the implication, and what should change now?
• Lumpectomy and adjuvant radiation should be considered for patients presenting with PAC of the breast are amenable to breast-conserving therapy.
• Although these tumors typically demonstrate “triple negative” receptor status, little is known about the benefit of chemotherapy.
• Given only limited information is available in the current literature regarding management and outcomes in patients diagnosed with PAC of the breast, we report another case of PAC of the breast which has thus far appeared to demonstrate non-aggressive behavior.
Introduction
Polymorphous adenocarcinoma (PAC) is defined by the World Health Organization (WHO) as an infiltrative salivary gland carcinoma (1), with 95% of PAC affecting the minor salivary glands (2). It is characterized by uniform tumor cells that exhibit architectural diversity (3).
PAC of the breast is a rare tumor with morphology similar to that of PAC of the salivary glands. Three cases were reported in 2006 (4). PAC was then added as a rare salivary gland-type tumor in the WHO classification of breast tumors (5). A fourth case was described in 2022 (6). The purpose of this case report is to describe a case of PAC of the breast that had a unique presentation. We present this case in accordance with the CARE reporting checklist (available at https://abs.amegroups.com/article/view/10.21037/abs-24-43/rc).
Case presentation
A 56-year-old woman presented with a superficial palpable nodule located immediately deep to the left areola in 2022. The nodule had been present and unchanged for one year prior to presentation. The patient has no history of previous malignancy. Family history was positive for breast cancer in her mother and prostate cancer in her father.
Physical examination showed a superficial marble-sized superficial mass just under the skin of the left areola that was well-circumscribed, mobile, and non-tender. Ultrasound of the left breast revealed a 5 mm × 4 mm hypoechoic structure located entirely within the dermal layer of skin, which suggested a benign skin lesion. The patient saw a plastic surgeon in early 2023, and excision of the left breast mass was performed under local anesthesia in the office.
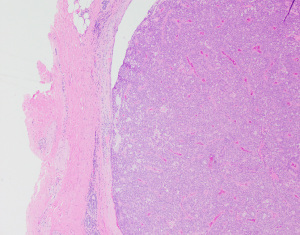
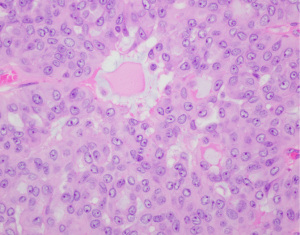
Pathologic review of the mass revealed a well-demarcated nodular lesion (Figure 1) showing a solid papillary growth pattern and microcyst formation with eosinophilic secretions of myxoid contents (Figure 2) measuring 0.8 cm and thought to be most consistent with salivary gland-type tumor favoring PAC, cribriform type. Margins were negative, with the carcinoma <0.5 mm from the closest resection margin. Mitotic activity was moderate (Figure 3) and there was no necrosis noted. Immunohistochemistry was positive for mammaglobin and GATA-3, and negative for the estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2). Slides were sent to an outside institution for second opinion and additional immunohistochemical stains were performed including cytokeratin (CK) 7 (diffusely positive), CK 5/6 (diffusely positive), S100 (diffusely positive), SOX10 (diffusely positive), vimentin (diffusely positive), epithelial membrane antigen (patchy staining), smooth muscle myosin 1 (patchy staining), calponin (patchy staining), CD117 (very focal weak staining), p63 (negative), auramine-rhodamine (AR, negative) and smooth muscle actin (SMA, negative).
Positron emission tomography-computed tomography (PET/CT) showed no evidence of metastatic disease. The patient was referred to a breast surgeon for re-excision lumpectomy given the extremely close margins as well as sentinel lymph node biopsy. She was offered but declined genetic testing. Final pathology from the re-excision showed no residual cancer. Sentinel lymph node was negative. Based on the size of the lesion and patient preference, adjuvant chemotherapy was not given. Based on current guidelines for breast-conserving therapy, adjuvant radiation was recommended and completed. No suspicious changes or evidence of malignancy were seen on mammogram at her 12-month follow-up. The patient continues to do well with no evidence of recurrent disease.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
The purpose of the present paper is to report an additional case of PAC of the breast and describe its unique presentation as a benign-appearing dermal nodule. There have only been four cases of PAC of the breast published to date. The current case is a unilateral triple negative breast salivary gland-type tumor, PAC of cribriform type diagnosed in a 56-year-old woman. Our immunohistochemical analysis is similar to the cases previously reported (4,6) in which the tumor stained strongly positive for CK 7 and was negative for P63, AR, SMA, ER, PR, and HER2. Like previous cases, our patient was node-negative. Unlike the previous cases, our patient’s breast mass presented as a benign-appearing nodule within the dermis of the areola and on pathology appeared well-demarcated.
Due to the rarity of these neoplasms, only limited data is available regarding treatment options and recurrence of the disease. Two of the three cases reported by Asioli et al. were treated with breast-conserving surgery and radiotherapy and the third underwent mastectomy; all three had axillary lymph node dissections without lymph node metastases identified. One of three patients developed liver metastases and died from widespread metastatic disease three years after presenting with a breast mass, while follow-up data for the other two cases is limited (4). The case reported by Franin et al. underwent adjuvant chemotherapy and radiation after breast-conserving surgery with no recurrence of the cancer being reported at one-year follow-up (6).
Complete surgical excision has been established as the primary choice of treatment for PAC of the salivary glands with adjuvant radiotherapy being considered in high-risk cases (7). Evans et al. reported there were no distant metastases or deaths due to the tumor in patients with PAC of the salivary glands who were treated with radical surgical resection (8). Given that breast and salivary glands are both tubulo-acinar glands with exocrine secretion, they share similar morphological features (9). This similarity contributes to their pathological processes of neoplastic transformation. Therefore, we expect most cases of PAC of the breast to respond similarly to PAC of salivary glands with the patient remaining clinically tumor-free at follow-up.
It is worth noting that another consideration for this patient presenting with a cutaneous lesion was the possibility of a skin neoplasm originating on the breast. Polymorphous sweat gland carcinoma is a rare, low-grade malignant tumor that typically presents as slow-growing dermal nodules (10). These tumors grow within the dermis and are characterized by a combination of histologic features, including cribriform patterns (10). However, papillary structures, trabecular formation, and solid lobular areas are not typical features of breast tumors, and serve to distinguish polymorphous sweat gland carcinoma from our case of PAC.
Conclusions
Although rare, PAC of the breast should be considered in the differential diagnosis of a breast mass. Breast-conserving therapy with lumpectomy and adjuvant radiation was successful in this patient who remains clinically tumor-free at 18-month follow-up. Therefore, the purpose of this case report is to add to the limited data available on PAC as a rare breast cancer variant, and to highlight its unique presentation as a benign-appearing dermal nodule.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://abs.amegroups.com/article/view/10.21037/abs-24-43/rc
Peer Review File: Available at https://abs.amegroups.com/article/view/10.21037/abs-24-43/prf
Funding: None.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://abs.amegroups.com/article/view/10.21037/abs-24-43/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- El-Naggar AK, Chan JKC, Grandis JR, et al. World Health Organization Classification of Tumours: pathology and genetics of head and neck tumours (4th edition). Lyon: International Agency for Research on Cancer (IARC); 2017.
- Mimica X, Katabi N, McGill MR, et al. Polymorphous adenocarcinoma of salivary glands. Oral Oncol 2019;95:52-8. [Crossref] [PubMed]
- Katabi N, Xu B. Polymorphous Adenocarcinoma. Surg Pathol Clin 2021;14:127-36. [Crossref] [PubMed]
- Asioli S, Marucci G, Ficarra G, et al. Polymorphous adenocarcinoma of the breast. Report of three cases. Virchows Arch 2006;448:29-34. [Crossref] [PubMed]
- Sinn HP, Kreipe H. A Brief Overview of the WHO Classification of Breast Tumors, 4th Edition, Focusing on Issues and Updates from the 3rd Edition. Breast Care (Basel) 2013;8:149-54.
- Franin I, Bubanović S, Milas I, et al. Polymorphous adenocarcinoma of the breast: A case report. Case Reports in Clinical Pathology 2022;9:24-26. [Crossref]
- Barnes L, Eveson JW, Reichart P, et al., editors. World Health Organization Classification of Tumours. Pathology and Genetics of Head and Neck Tumours. Lyon: IARC Press; 2005.
- Evans HL, Batsakis JG. Polymorphous low-grade adenocarcinoma of minor salivary glands. A study of 14 cases of a distinctive neoplasm. Cancer 1984;53:935-42. [Crossref] [PubMed]
- Pia-Foschini M, Reis-Filho JS, Eusebi V, et al. Salivary gland-like tumours of the breast: surgical and molecular pathology. J Clin Pathol 2003;56:497-506. [Crossref] [PubMed]
- Suster S, Wong TY. Polymorphous sweat gland carcinoma. Histopathology 1994;25:31-9. [Crossref] [PubMed]
Cite this article as: Grigorian D, Candell L. Polymorphous adenocarcinoma of the breast: a case report and review of the literature. Ann Breast Surg 2025;9:15.


